Clinical Protocols and Therapies
The key idea of the CLEAR project is to allow hospitals and clinical centers to develop, validate and assess the home therapies assigned to the specific home users.
Below you can find, for each disease treated, two items:
- Neurological
- Musculoskeletal
- Pneumonic diseases
Cognitive disease - FPING (Fundació Privada Institut Guttmann) [ES]
Description of the scenario
1 - Characterization of the patient
Jordi is 49 years old and he is retired. He had a stroke, and suffers from a left hemiplegia and cognitive impairments. He has problems with his attention, visual perceptive and memory. Before his stroke he lived in his own house. His wife died 2 years ago. His daughter lives with her family in the same street. Jordi was admitted in Guttmann 3 months after the stroke because of the cognitive problems.
2 - Description of the traditional treatment
Single-mode treatment or treatment in a group of maximum 3 people, using paper and pencil tools which the therapist provides to each patient during the session.
This requires the previous identification of the appropriate exercises, photocopy the required material, the manual correction of the paper and pencil executed
exercises and the manually recompilation and storage of the obtained results. Treatment: 2 days per week. Transport to the hospital (by ambulance, or private transport).

3 - Patient Recruitment
Jordi was admitted in Guttmann 3 months after the stroke because of the cognitive problems. He started with physiotherapy, occupational therapy and neuropsychological rehabilitation. Because of the brain damage he will have more probabilities to develop an earlier cognitive aging due to the cerebral insult. With the Clear system there is an opportunity to continue the cognitive rehabilitation at home. Therefore, Jordi is invited to use the CLEAR system. In the last weeks of his stay in Guttmann Jordi will learn how he has to use the system. His daughter will also be trained in using CLEAR, because she offered to help her father with his exercises. Jordi will receive a login code to enter the CLEAR system, and the therapists will teach him where to find the exercises he has to perform.


4 - Description of the tele-rehabilitation program or the tele-care for the patient
The exercises Jordi has to perform have simple, clear and short instructions. Jordi is already familiar with the exercises because he performed them also during his stay in the Guttmann. An assessment will be done before discharge in order to know the current cognitive status. Based on this profile the neuropsychologist will plan an individual therapy plan to improve and to maintain visual perceptive and memory skills when Jordi is at home. For the following 3 months the cognitive exercises will be provided with the CLEAR system. At home, Jordi has a computer with web cam and access to internet. The computer has an adapted mouse, and includes a headphone for the tasks in which sounds are important.


5 - Description of a tele-reabilitation session
Jordi can login to receive a set of specific tailored tasks, which have to be performed 5 times a week in sessions of one hour per day. At the end of each exercise Jordi will receive a feedback of the performance (number of correct answers, total score). There will be positive reinforcement within this feedback, in order to try to motivate the patient. In addition, the information concerning his performance (time to finish a task, correct answers, type of errors) will be sent to a server located in Guttmann.
6 - Description of the interaction with the therapist
The neuropsychologist will have instant access to Jordi’s data and weekly will monitor Jordi’s progress. Moreover, a videoconference contact will take place with the patient. Based on the task performance and the videoconference contact, the neuropsychologist will remotely plan the next sessions which can be performed at home. At the beginning, Jordi may need some help from his daughter. Due to memory problems Jordi may not remember the password or the logical steps to start the treatment sessions. Together with the therapist his daughter will try to motivate Jordi to perform the exercises.
7 - Description of the therapist session
The therapist connects to the platforms and examines the performances of the patient in the previous sessions. Based on these results, the therapists schedule an adapted rehabilitative therapy. The therapist assigns exercises adapted according the deficits of the patients and the results obtained so far. When Jordi opens his cognitive exercises module, begins to undergo the treatment.
8 - Description of the advantages the programs has for the patients
During the cognitive telerehabilitation treatment, Jordi will receive during a 12-week period, specific cognitive task according to his neuropsychological impairment. As described in the scenario, main cognitive deficit are attention, visual processing and memory. Thanks to this remote treatment, the patient has had the opportunity to continue seeking a personalized and individualized therapy schedule by a therapist tailoring the treatment to their specific deficits without having to afford transportation or wasting time traveling to the Hospital. Also now feels that leverages the time spent at home and has improved his concentration and memory.
9 - Description of the advantages this program has for the therapist
This program provides the neuropsychologist responsible of Jordi’s therapy, have in a clear way the performance of your patient. Similarly, it is much easier to communicate with him through the functionality provided by the platform. You can, thus, establish an intensive personalized and individualized treatment, asynchronous, saving time and improving accuracy of treatment.
10 - List of the participants at the definition of the scenario
| Name participat | Profession | Company | Contact e-mail |
|---|---|---|---|
| Pablo Rodríguez | Neuropsychologist | FPING | prodriguez@guttmann.com |
| Rocío Sánchez-Carrión | Neuropsychologist | FPING | rsanchezcarrion@guttmann.com |
| Eloy Opisso | Engineer | FPING | episso@guttmann.com |
Clinical Protocol
Here below the protocol on cognitive disabilities designed by FPING (Fundació Privada Institute Guttmann) is described.
Overview
Patients with cognitive impairment due to acquired brain injury (traumatic brain injury or stroke) will benefit from this intensive, monitored and prolonged cognitive treatment.
Additionally, a large number of patients need to continue cognitive treatment after the hospital discharge in spite of the geographical barriers that may exist.
On the other hand, the neuropsychologist in charge of the treatment will have access to several patients and will offer them an individualized therapeutic plan for their cognitive
treatment. Additionally, the neuropsychologist will need to monitor patients results and will analyze whether their performance is as it was predicted.
Thus, both patients and neuropsychologists will be the users of this telerehabilitation service.
Conventional cognitive treatment is usually very heterogeneous regarding number of sessions, number of tasks and performance. Besides those parameters are uncollected and because of
this unable to be controlled. This heterogeneity drastically reduces the opportunity to collect critical mass and experience concerning the therapeutic strategy used. As a consequence
the conventional cognitive treatment is often not actually satisfying either for the patient or for the neuropsychologist. Computerized cognitive tasks have shown better outcomes as well
as being a better tool to collect data to further analysis. Previous experiences have shown the feasibility of physical telerehabilitation program.
The service provided through the Habilis platform will consist of a cognitive telerehabilitation service and will be implemented locally in the Clinical Centre, providing individualized
and systematic cognitive treatment to actual patients with the supervision of one therapist (neuropsychologist or occupational therapist) for each seven patients. This treatment will be
focused on attention, memory and executive functions. Besides the telerehabilitation service will be installed in an amount of patients’ home.
Most of the patients perform the treatment on hospital in a range of session since two to five per week. The period of treatment in hospital depends on the clinical criteria and is decided
by the entire clinical team. All sessions extends around one hour.
Patients will undergo in home scenario, five day a week one-hour cognitive treatment sessions during two months.
Both treatments will be planned by neuropsychologist in a personalized, systematized and monitored manner.
Patients will undergo two main neuropsychological assessments one at the beginning and the other one at the end of the treatment program. Improvement in different test will indicate whether
therapeutic goals have been reached or not.
The rationale for providing this cognitive rehabilitation via the Habilis service is that treatment is much more structured, can be better monitored and adapted according to the individual
patient’s problems and transferring the treatment to the home or daily healthcare situation enabling the patient to train during longer periods of time and much more intense. As such it is
expected that it makes treatment much more effective than the convention cognitive behavioural treatment.
Target Patient Group
Population (base)
The target patient group will be patients with cognitive disability due to acquired brain injury, such a traumatic brain injury (TBI) or stroke, receiving neurorehabilitation treatment in the Clinical Centre as inpatient or outpatient. Each patient will receive the cognitive telerehabilitation treatment during 12 weeks.
Inclusion criteria
The exclusion criteria are:
- patients with language impairment (aphasia);
- patients with sensory or motor disability that prevent or hinder the use of computer peripherals;
- patients presenting with psychiatric disorders.
Admission and baseline assessment
The patients undergo a first neuropsychological assessment prior to any inclusion to the treatment program.
During the stay in the Centre or during external consultation, cognitive impairment in attention, language, memory and executive functions will be detected by a specific neuropsychological
assessment. This assessment takes place in two one-hour sessions. Based on the results of this assessment, the neuropsychologist will establish patient’s impairment profile and will define
a personalized therapeutic plan.
The Neuropsychological assessment covered the major cognitive domains (language, attention, memory and learning, and executive functions). Language tests
assess repetition of words, confrontation naming, and verbal comprehension. Measures of attention included Digit Span Forward, Trail Making Test-A, and Stroop Test (word-colour condition).
Memory and Learning was assessed with Digit Span Backward, Letter-Number Sequencing, and /Rey Auditory Verbal Learning Test/. Executive functions was assessed with the Wisconsin Card
Sorting Test, Trail Making Test-B, Stroop Test, and verbal fluency test (COWAT). Standard values of each test or scale are used to assess the neuropsychological impairment of the patients
and whether to include them to the treatment program or not.
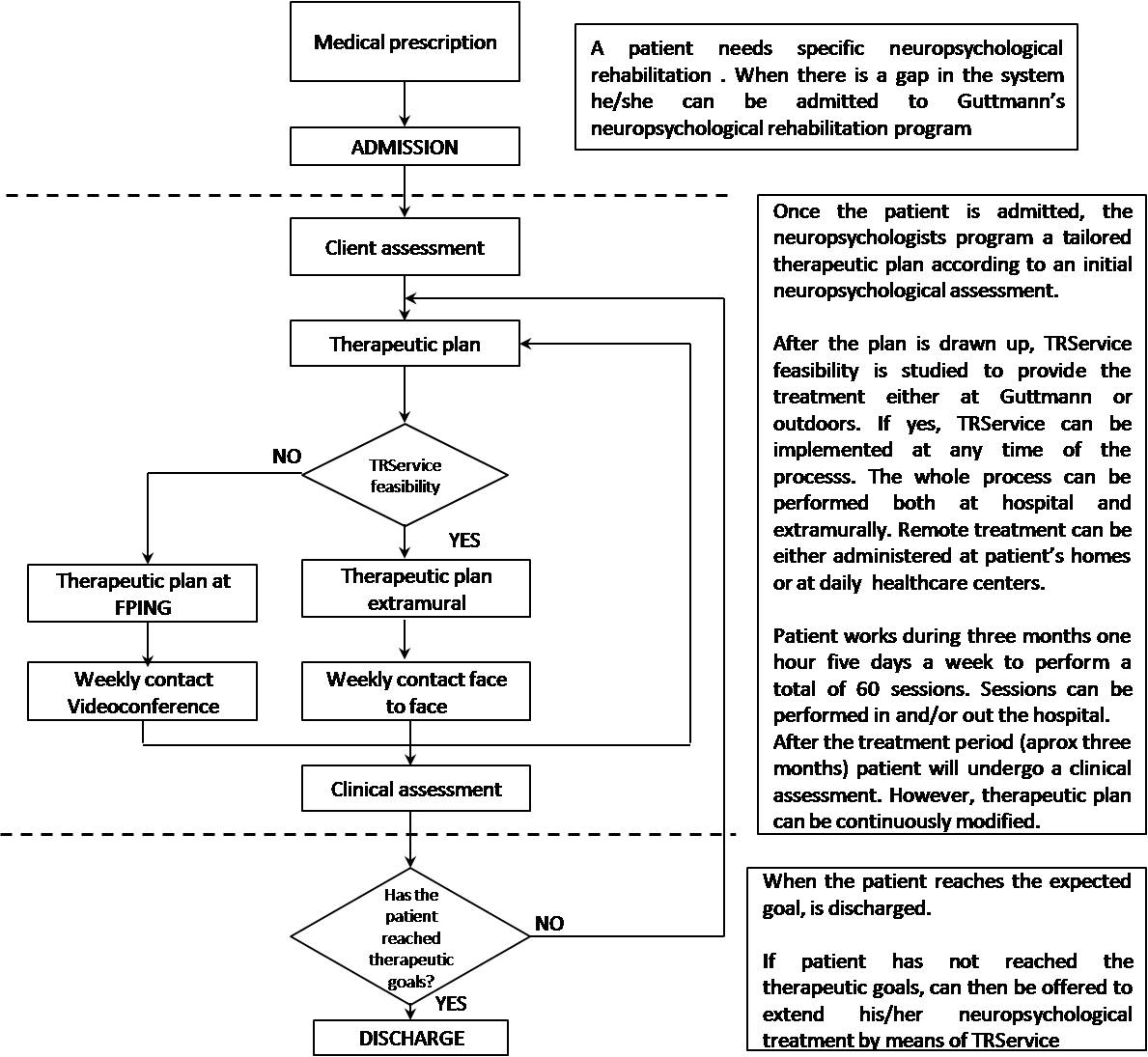
Cognitive treatment in all cases would start at Clinical Centre, however TR service feasibility is analyzed for each individual at the beginning of the cognitive rehabilitation treatment.
If the patient and its personal situation fulfil the requirements, then they can be moved to tele-rehabilitation treatment at any period of the program. In other words, patients have to
meet the inclusion criteria and they must be both clinically stable and outpatients. Most of the patients who need cognitive treatment often also need physical rehabilitation. When both
treatments can be performed outdoors, it is actually the proper time to transfer the cognitive rehabilitation into a remote system.
Treatment protocol
Treatment will take place, intensively, during a 12-week period. Each patient will be enrolled in 5-day week sessions, for one hour, neuropsychological rehabilitation program.
During this customized weekly therapeutic plan the patient will perform daily sessions (Monday to Friday) of 45 to 60 minutes. The time to set treatment guidelines will be approximately
30 minutes. A 30 minutes videoconference interview with the patient, will take place every week, to collect information about the adequacy of treatment. In all cases the therapy will be
based on initial deficits and functional residual capacity detected by neuropsychological exploration, and will be weekly adjusted based on information obtained from the patient and their
caregivers, through interview (hospital) or videoconference (home). All exercises, and its level of difficulty, will be defined individually for each patient taking in to account his/her
cognitive profile. Each patient will have a code and a password to enter the neuropsychological rehabilitation program in order to access, remotely, to his personalized rehabilitation
session.
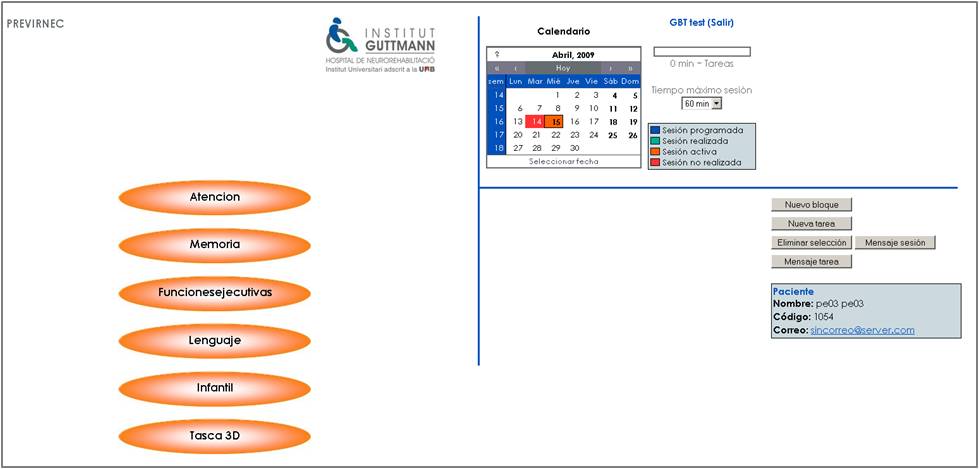
The Habilis service is conceived as a tool to enhance the rehabilitation, strengthening the relationship therapist-patient, individualisation of treatment, monitoring of results
and performance of the tasks from the patient's home, reducing the costs of displacement and distortion on activities of daily living of the rest of the family, carrying out tasks in a more
environmentally friendly and the socialization of people with disabilities. The platform comprises a user interface (patient) and a therapist interface. Through the user interface, the
patient each time the scheduled task on the level of difficulty and, once executed, the data are sent to the server. Depending on the outcome of the task performed, the system sends a
series of parameters of the scheduled task, or a version of the same task, adjusted level of difficulty, if the number of errors or successes is not consistent with the initial forecast
of the therapist, making this attempt to set up twice. The interface allows pattern therapist working sessions for each patient and observe the results of each task. From any of these
interfaces can have a videoconference between the therapist and the patient or their caregivers.
Neuropsychologist will be in charge of monitor the treatment and supervise patients’ performance, during the 12-week treatment, once a week. According to the results, the neuropsychologist
will plan the exercises to be performed the following week.
The program provides an interface to elaborate therapeutic plans, with a library of tasks, for each cognitive function and sub-function. They can select the task, the level of difficulty
and the parameter by which the level of difficulty is auto-adjusted. The application provides also another interface for visualization of results where the therapists can see (colour coded)
whether the session has been or not, totally or partially, realized, and whether the task were or not in the therapeutic range (based on the percentage of right responses), directly, after
any of the two trials of auto-adjustment of the level of difficulty or it was out of the therapeutic target.
Both intramural and extramural cognitive rehabilitation are continuously monitored by the neuropsychologist in order to fine tune the treatment according to the patient needs. Extramurally,
the neuropsychologist contacts the patient through the CLEAR videoconference module. This contact is prior agreed by the neuropsychologist and the patient and programmed every week.
Nevertheless, patients are welcome to contact to the professional in case of any inconvenience by the same means.
Patients are encouraged by the neuropsychologist to comply with the proposed treatment within the whole program. This is done during the periodical contacts.
Patients with cognitive impairments such as attention, memory or executive functions have often behavioural problems. In case of a bad compliance to the treatment, patients are contacted up
to three or four times to make them change their attitude towards the treatment. Talking sessions with them and family are the most common approaches to solve the problem. If this fails,
then the patient is excluded from the cognitive rehabilitation program.
Outcome assessment
Outcome parameters
Main study parameter/endpoint
(I) MAIN VARIABLE: The main variable is the clinical response with respect to the treatment based on the exploration of attention, memory and executive functions, following
the exploration protocol of Institut Guttmann.
Cognitive functioning was assessed at baseline and post-treatment (aprox. 3 months). Cognitive assessment consisted of selected tests of attention, memory, execute functions and language.
Cognitive assessment took about 1 hour and a half.
Cognitive assessment tools are detailed below:
- Digits forward WAIS-III: Digit Span (DS) requires the immediate verbal recall of a series of numbers in the exact order as presented. Outcome measures were maximum number of digits correctly recalled.
- Trail Making Test part A: This test measures visual-conceptual and visual-motor tracking. In the first test, 25 numbers are presented inside circles. Participants are required to connect the numbers in ascending order (i.e. 1-2-3- etc.) as quickly and as accurately as possible. This test assesses the basic ability to hold attention on a simple task.
- Stroop Test: the Stroop effect is a demonstration of the reaction time of a task. When the name of a color (e.g., "blue," "green," or "red") is printed in a color not denoted by the name (e.g., the word "red" printed in blue ink instead of red ink), naming the color of the word takes longer and is more prone to errors than when the color of the ink matches the name of the color.
- Symbol Digits: is a neuropsychological test sensitive to brain damage, dementia, age and depression. It isn’t sensitive to the location of brain-damage (except for damage comprising part of the visual field). It consists of (e.g. nine) digit-symbol pairs followed by a list of digits. Under each digit the subject should write down the corresponding symbol as fast as possible. The number of correct symbols within the allowed time (120 sec) is measured.
- Popelreuter: This test shows the subject a mixed picture with some figures. He should be able to discern which separate images are present in that drawing.
- Digit backwards WAIS-III: requires the immediate recall of a number serial in reverse order. The series of digits for both forwards and backwards become progressively longer as the participant correctly recalls the series. Measures recorded are maximum number of digits correctly recalled.
- Numbers & Letters WAIS-III: In these test patient should repeat a sequence (e.g: Q-1-B-3-J-2) but place the numbers in numerical order and then the letters in alphabetical order.
- Rey Auditory Verbal Learning Test (RAVLT): This test assesses short term memory, retrieval of information from long-term memory (delayed memory) and storage of information in long-term memory (delayed recognition). There are two parts to this test. In the first part, participants are presented with a list of 15 concrete words (which they are asked to memorize). The list is presented 5 times in total, and the participant is required to recall as many words as possible in one minute following each presentation (immediate recall). Twenty minutes after the presentation of the last trial, participants were required to recall as many words as possible from the original list (delayed verbal recall). The second part of the test involved recognition of the original list of words. Specifically, words from the original list and distracter words are presented. Participants are required to respond "yes/no" as quickly as possible as to whether the word was in the original list (delayed recognition). The outcome measures were total trial score learning rate and delayed memory recall score.
- Trail Making Test part B: Participants are required to connect the numbers in ascending order, but alternating between letters (in alphabetical order), as quickly and as accurately as possible. The outcome measures were time to completion and average connection time.
- Cubes of WAIS-III: The subject must make constructions using cubes to match patterns. These test measures visoconstruction processing and problem solving.
- Phonological verbal fluency PMR: It is a measure of a verbal fluency, which refers to an individual’s capacity to produce a sustained stream of spontaneous speech. The participant is required to name as many words as possible, beginning with a specific letter (most commonly P, M, and R for which word naming is relatively easy) within one minute. The measured outcome was the number of words produced.
- Interference of the Stroop: This is a test index that calculates the interference in the performance experienced by the subject after reading the list of words, colors, and words written in different color.
- Wisconsin Card Sorting Test: It has been considered a measure of executive function because of its reported sensitivity to frontal lobe dysfunction. As such, the WCST allows the clinician to assess the following "frontal" lobe functions: strategic planning, organized searching, utilizing environmental feedback to shift cognitive sets, directing behavior toward achieving a goal, and modulating impulsive responding. Initially, a number of stimulus cards are presented to the participant. The shapes on the cards are different in color, quantity, and design. The person administering the test decides whether the cards are to be matched by color, design or quantity. The participant is then given a stack of additional cards and asked to match each one to one of the stimulus cards, thereby forming separate piles of cards for each. The participant is not told how to match the cards; however, he or she is told whether a particular match is right or wrong. During the course of the test the matching rules are changed and the time taken for the participant to learn the new rules, and the mistakes made during this learning process are analysed to arrive at a score.
Secondary study parameters / endpoints (if applicable)
(II) Use, satisfaction, usability and ICT covariables will be considered for the technical assessment of the telemedicine system. In our case, in addition to this measure of satisfaction,
usability, design, learning, acceptance and usefulness of the system, data will be automatically gathered regarding system usage. Therefore, these variables should measure:
- The quality of the system (efficiency, effectiveness, usefulness and accuracy), reliability of the system (reliability, security, interoperability and ease of repair and maintenance)
- The usability of the system (ease of use, design, satisfaction, user control, support, learning and acceptance)
- The use of the system (who is using the system, how, how often and in what context) by an automatic system that will monitor parameters at any time as the start / end of session, access to a patient’s data, start / stop a video, send a message, and so on.
(III) TASK PERFORMANCE covariables: collect the number of errors and successes of each task execution. For each one, the team of therapists responsible for their design considered a range of success as therapeutic. A qualitative analysis will take place, based on the number of tasks performed in therapeutic range for each patient and regression studies based on the direct obtained scores for each task. Both comparison approaches will be used to assess the usefulness of the task management system implemented in the platform.
Outcome measures
At the end of both intramural and extramural cognitive treatment (after 3 months), neuropsychological assessment will again be administered to each patient, in order to analyze cognitive improvement. At that point, patient is either discharged if the expected clinical goals are reached or his treatment is prolonged by means of TR service. Patients with cognitive impairments such as attention, memory or executive functions have often behavioural problems. In case of a bad compliance to the treatment, patients are contacted up to three or four times to make them change their attitude towards the treatment. Talking sessions with them and family are the most common approaches to solve the problem. If this fails, then the patient is excluded from the cognitive rehabilitation program.
Withdrawal
Subjects can leave the study at any time for any reason if they wish to do so without any consequences. The clinician can decide to withdraw a subject for urgent medical reasons. The cognitive neuro-rehabilitation exercise program is estimated to have minimal risk as patients are trained in the exercises presented during the neuropsychological treatment.
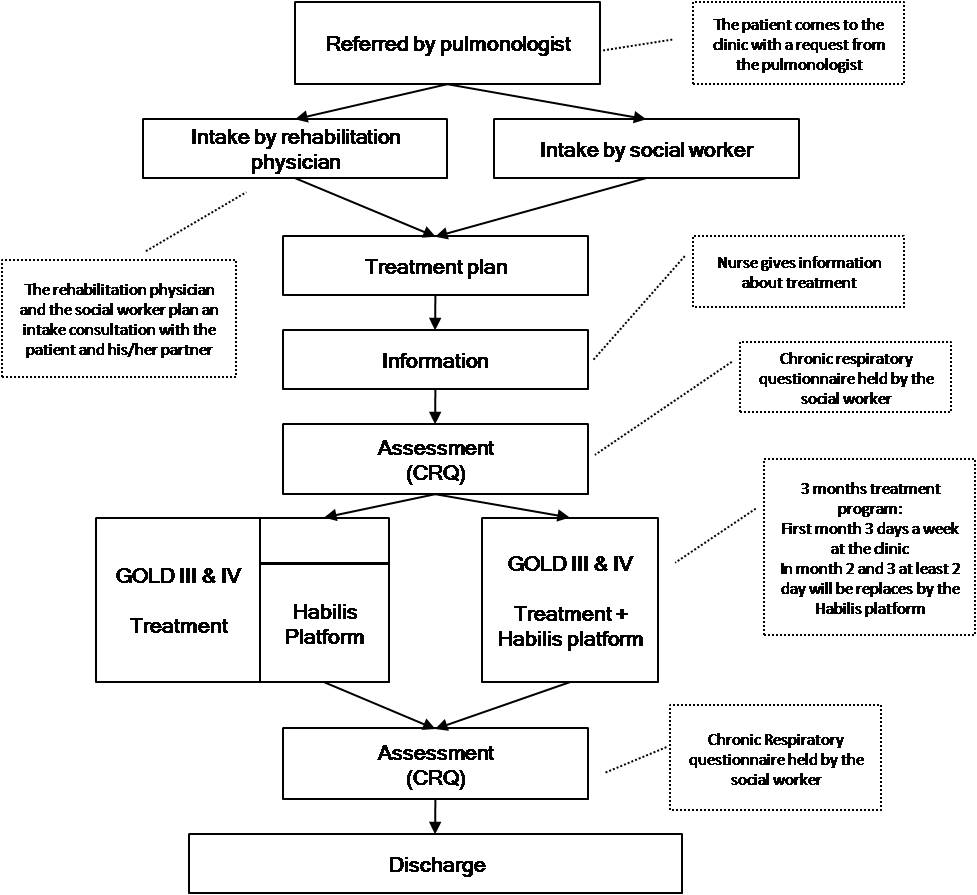
Protocol flow chart
Upper limb paresis after stroke - AUSL11 (Azienda Unità Sanitaria Locale 11 Empoli) [IT]
Description of the scenario
1 - Characterization of the patient
Piero is a 66 years old man who had stroke 4 months ago with residual left hemiparesis. Piero lives in Empoli with his family consisting of his wife and a 25 years old son. He has been discharged at home by the rehabilitation hospital of the AUSL11 3 months ago, and subsequently treated at the rehabilitation community service of Empoli.
2 - Description of the traditional treatment
Piero is almost at the end of his rehabilitation program. He attended the rehabilitation community service of Empoli 3 days a week for two hours sessions for 3 months.
Physiotherapists provided a therapy plan for Piero to regain the use of stroke-impaired limbs, teach compensatory strategies to reduce the effect of remaining deficits,
and establish ongoing exercise programs to help him to retain the newly learned skills. As time passed by, and the motor task were consistently learned by Piero. Thus,
the role of physiotherapists was reduced passing from that of a trainer to that of a supervisor and Piero was encouraged to work more and more autonomously.
Eventually Piero had a nice recovery of locomotion and is now able to walk independently without assistive devices both at home and outside. However, the upper limb function,
although markedly improved, still presents significant limitations which causes difficulty with everyday activities. For this reason, he tends to avoid using impaired limb,
and compensate with the controlateral arm. Physiotherapists are worried that Piero could loose the benefits of the rehabilitation treatment if he stops practicing the skills
learned during the rehabilitation period.
3 - Patient Recruitment
Physiotherapists think Piero could maintain the paretic upper limb function or even improve more if he continues to practice within the framework of a long term task-oriented treatment. Therefore Piero was proposed to continue on practicing after discharge both at home and by using the SW Habilis in specialized ‘kiosks’. The kiosks allow him to practice outside the clinic, but still under the remote supervision of his therapists. In this way he would be able to expand the period of practicing functional tasks with his arm, while at home.
4 - Description of the tele-rehabilitation program or the tele-care for the patient
Piero receives detailed explanation of how the long term task-oriented treatment works. The role of the physiotherapists (patient education and updating treatment plan),
the importance of home practice (regularity, intensity of training) and the role of the kiosk (for both practice and assessment by the Habilis platform) are emphasized.
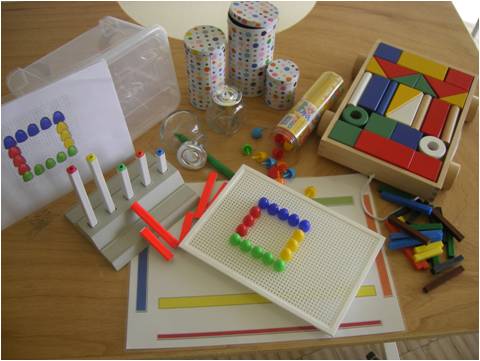
Subsequently, Piero is instructed, within the community rehabilitation setting of the Local Health Authority in Empoli, to practice a given list of therapeutic exercises aimed
at improving upper limb function by using rehabilitation devices provided by AUSL11 (different shape and size objects to manipulate, puzzles, printed paths to follow with pens
of different shape and size).

In addition, he is trained to use patient Habilis platform which he will find in the most convenient kiosk near his home. His wife is associated to the entire process of training to instruct her on the best way to assist Piero, if needed.
At the end of the instructional period (three 2-hour training sessions) Piero are given:
- All the rehabilitation devices needed for practice at home (“rehabilitation suitcase”);
- The list of the exercises to perform at home, with specification of frequency and intensity of exercise training (“home program sheet”);
- A logbook where indicate the execution of the given tasks;
- The weekly time schedule in which the kiosk will be available for him.

Piero attends the kiosk 2-3 times a week and practice the same home exercise while assisted by the patient unit of the Habilis platform. He is instructed not to bring the “rehabilitation suitcase” with him since the entire set of rehabilitation devices is available in the kiosk, ready for him. Piero performs his exercises and record them the as instructed.

Kiosks are supervised by volunteers which assure opening/closing the door of the kiosk, cleaning the environment, maintaining the equipment in proper order and ready-to-use. His wife assisted Piero during the first two training sessions in kiosk, but subsequently it was no longer necessary.

5 - Description of a tele-reabilitation session
Piero enters user name and password. The platform sends a personalized message that indicates the exercises he has to execute. Piero choose an exercise and the tutorial video with the explanation to execute appears. Piero finds the proper training devices (which are alla valilable in the kiosk) and execute the exercise in front of the webcam. Thus, the exercise is video-recorded. He can also add some comments for the physiotherapists, if necessary. When completed the first exercise he selects the following exercises until the end ot the scheduled session program. Then Piero logs out and leaves the “kiosk”.
6 - Description of the interaction with the therapist
From the “doctor unit” of the Habilis platform located within the AUSL11 Rehabilitation service, physiotherapists review off-line patient’s performance at least once a week. Physiotherapists via teleconference may also reassess Piero performance and/or give him advice for improving practice. Piero may also request advice from the physiotherapist via Habilis platform. Physiotherapists may schedule for Piero an appointment for a visit in the AUSL11 Rehabilitation service if the treatment plan need to be revised (and new skills have to be learned) or a visit with a MD is necessary for the occurrence of adverse clinical events.
7 - Description of the therapist session
Physiotherapists connect to the platform by the “doctor unit” of the Habilis Platform. The platform shows if there are exercises recorded by Piero to be evaluated. The physiotherapists can observe videos of the exercises at high speed, and rate their execution giving a score. The score is useful to define Piero’s improvements. If necessary, physiotherapists assign Piero new exercises modifying the list of exercises (and hereinafter the tutorial) that Piero will find at the kiosk in the next scheduled session. In addition, the Habilis platform gives the physiotherapists the possibility to verify the adherence of the patients to the exercise program. If Piero misses a two or more session, physiotherapists contact him to verify the problems causing the low adherence. If necessary physiotherapists schedule for Piero an appointment for a visit in the AUSL11 Rehabilitation service if the treatment plan needs to be modified or a visit with a MD is necessary for the occurrence of adverse clinical events.
8 - Description of the advantages the programs has for the patients
Piero likes the treatment because he finds it effective. In addition, he finds convenient the treatment program because it allows him to exercise everyday at home without going to the hospital which is located far form home (about 15 km). His kiosk is located near home and allows him to maintain contact with physiotherapists. He knows physiotherapists revise his videos with the exercises he has performed at the kiosk. Piero finds that attending the kiosk and practicing with the Habilis platform is not boring. Indeed, he find interesting to learn the use of the computer. Finally, he often meets other persons in the kiosks with whom he share his experience.
9 - Description of the advantages this program has for the therapist
At the beginning, to realize a video, the team defined a library of exercises. Before the discharge from the community rehabilitation service, the therapist spent more time with Piero to teach him the exercises to perform at home and at the kiosks and how to use the platform. After that the therapist learned both how to watch the video at high speed (using the tools provided by the platform) and how to visualize more exercises at the same time. The time he spends to watch the exercises with respect to the time Piero spends to record them is reduced of a quarter. By using the functionalities where the summary of the score of the patients is, he/she can manage the patients in a more effective and systematic way. This gives AUSL11 rehabilitation services the opportunity to treat more patients, and at the patient to exercise for a longer time, with better results.
10 - List of the participants at the definition of the scenario
| Name participat | Profession | Company | Contact e-mail |
|---|---|---|---|
| Benvenuti Francesco | MD | AUSL11 | f.benvenuti@usl11.tos.it |
| Taviani Antonio | MD | AUSL11 | a.taviani@usl11.tos.it |
| Corsi Sara | Physiotherapist | AUSL11 | sarackx@hotmail.com |
| Nesi Barbara | Physiotherapist | AUSL11 | b.nesi@usl11.tos.it |
| Cappena Veruscka | Physiotherapist | AUSL11 | veruscka.cappena@alice.it |
Clinical Protocol
Here below the protocol on functional impairment of upper limb after stroke designed by AUSL11 is described.
Overview
One of the major challenges for the National Health System is coordinating continuous care for patients with chronic consequences of stroke. Stroke has a high incidence rate in developed
countries (2.2/1000). Although mortality rates are elevated in the first month after the acute event (20-30%), the percentage of those who survive is high (to one year is 60-75%; to 3
years 40-68%). It is estimated that more than 35% of the patients survive longer than 10 years. Therefore the prevalence of chronic stroke survivors is high (500-800 cases per 100.000
inhabitants).
The functional and neurological recovery happens more rapidly from the 1st to the 3rd month after the acute stroke, but continues even afterwards as demonstrated in some studies.
However, the functional recovery is often incomplete. In fact, 35-40% of the survivors has serious disability while a high but not defined percentage of cases shows milder disablements
that influence mobility, advanced activities of the daily life and the quality of life. Therefore stoke is one of the principal causes for disability among the senior population.
Arm functions play a fundamental role for manipulation, reaching and interaction with the environment. The upper limb is involved in a large variety of tasks which require the limb to
produce different joint configurations and different timing and sequencing of arm movement. When upper limb is impaired, an important characteristic of human functioning is lost.
It has been reported that only 5-20% of patients regain full arm and hand function after stroke while 20% remain with no functional use. It is typically reported that the main part of
the potential recovery level of the upper limb takes place in the first three months after the stroke. However, studies about training and forced use training started also more than
one year after stroke showed considerably recovery even after the early three-month period. This contradiction can be at least partially explained. Although the cerebral lesion is the
primary cause, there is a sufficient quantity of data in published literature that leads to the conclusion that the disability due to the stroke is made worse by the additive effect
of inactivity. Indeed Carr and Shepherd state that poor recovery may reflect an insufficient and time-limited therapeutic intervention for the upper limb.
The core idea is to integrate hospital rehabilitation, with home practice and with an intermediate moment in the so called “kiosk”. The “kiosk” is intended to provide patients a common
environment where they can socialise, perform continued and intensive practice and receive the necessary supervision and assessment by health professionals by the use of the Habilis
platform.
The Clinical Centre will be responsible to define the personalised treatment plan, updated with an incremental level of difficulty and progression if necessary. In the hospital setting
patients will be instructed to practice specific rehabilitation tasks and to use the Habilis platform.
Patients, when able to perform the home tasks and use the Habilis platform, will be discharged and requested to repeat the learned tasks every day at home and at least twice a week in
a “kiosk”. Very simple rehabilitation devices will be used, which are low cost and easily available in the community (different shape and size objects to manipulate, puzzles, printed
paths to follow with pens of different shape and size). The appropriate training material for home practice is given to the patient by the physiotherapist (“training suitcase”).
If necessary, a care giver is also instructed to assist the patient in his/her home exercise sessions.
The “kiosks” will be located and run by social clubs or voluntary association. Each “kiosk” will be equipped with at least two client platforms, the same training material used at home
and other opportunities of computer based exercises. A client platform will not be dedicated to a single patient, on the contrary every platform will be able to serve each patient properly
(according to a personalised rehabilitation protocol) once identified, by means of an identity smart card. Expected outcomes of tele-rehabilitation treatment must be considered with
two different perspectives, the patient and the organization one.
From the patient’s perspective, a better functional outcome is expected since the time of practice is significantly increased, in comparison with time dedicated in usual inpatient care
where rehabilitation services are provided in the sub acute phase after stroke within a strict time-frame of intervention. However, repetitive practice of an action, both with and without
supervision, is a necessary component for acquiring or reacquiring skill in that action. Thus, the combination of home and kiosk practice with clinical practice within rehabilitation
services may provide an unique scenario for enabling patients, once movement patterns are learned, to strengthen muscles specifically and to enable stable movement patterns to be
modified as necessary according to environmental and other demands. In addition, in the chronic phase of the disease the beneficial effects of rehabilitation reached during the acute
and sub acute stages of the disease tends to fade away as time passes by due to inactivity. Thus, short and frequent maintenance cycles are often requested by chronic stroke survivors.
These cycles of treatment have a very limited and short term effects on health and functional status and influence only marginally the long term disabling process, while generating
illusion of care and fostering dependence of patients on rehabilitation systems. The combination of home and “kiosk” practice, with the supervision of hospital rehabilitation services,
may provide the unique opportunity for patients for maintaining/improving function even for a long time after stroke.
The first expected outcome is the reduction of pressure by individuals with chronic stroke disabilities on the rehabilitation services which are already overcrowded because of the
high incidence of acute disabilities caused by the aging of the population. However, the most important expected outcome would be the implementation of a “chronic care model”(21)
which, if successful, will be implemented in other chronic disabilities other than stroke. The interaction between hospital, home and “kiosk” activities can provide a new scenario
to foster productive interactions between patients that take an active part in their care and providers backed up by resources and expertise.
In particular the Habilis service allow the implementation of the following specific strategies:
- empower and prepare patients to manage their health and health care;
- assure the delivery of effective and efficient clinical care and self management support;
- promote clinical care that is consistent with scientific evidence and patient preferences;
- facilitate transmission of patient data to facilitate efficient and effective care;
- create culture, organization and mechanisms that promote safe and quality care for chronic patients;
- mobilize community resources to meet the needs of patients and their families.
Target Patient Group
Population (base)
Patients with chronic stroke who meet the following inclusion/exclusion criteria (that will be evaluated in a preliminary clinical multidimensional assessment).
Inclusion criteria
The inclusion criteria are:
- Time from stroke >3 months;
- Age > 40 years;
- Presence of minimal residual function of the paretic limb (Enjalbert Scale>4).
Exclusion criteria
The exclusion criteria are:
- Severe dementia (Mini Mental State Examination <15), aphasia, apraxia, blindness, deafness which prevent understanding and execution of rehabilitation tasks;
- Symptomatic congestive hearth failure (II-V NYHA), unstable angina, pulmonary disease which requires oxygen therapy, recent (<3 months) miocardial infarction or hospitalization, pain which interfere with exercise, poorly controlled (diastolic blood pressure > 95 mmHg, systolic blood pressure >160 mmHg);
- Any other documented medical condition considered to contraindicate a long term exercise program by the medical doctor;
- Unable to reach the “kiosk” alone or with the assistance of a caregiver;
- Refusal to signing the informed consent form.
Admission and baseline assessment
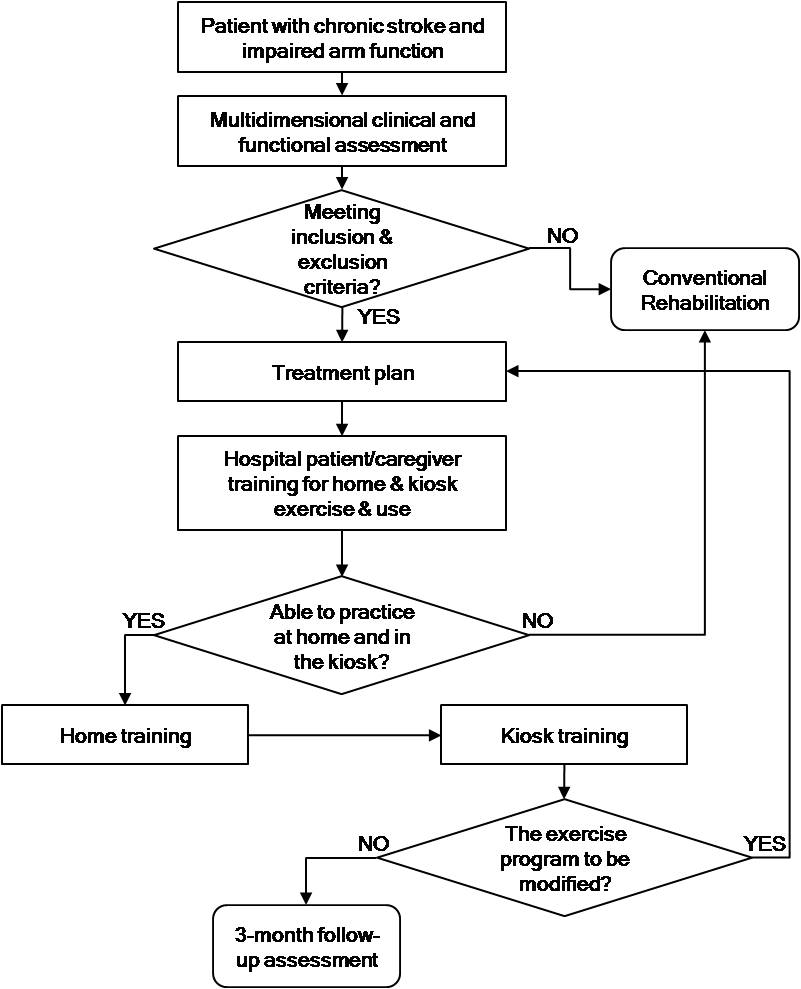
Patients with stroke and residual impaired upper arm function will be referred for treatment by general practitioners, hospital specialists and other rehabilitation facilities.
After the initial structured medical and functional evaluation the criteria for inclusion and exclusion are verified.
The multidimensional medical and functional evaluation will include the assessment of:
- Demographic and anthropometric characteristics;
- Living and social characteristics;
- Stroke characteristics (time of stroke, affected side) and comorbidity (Cumulative Illness Rating Scale);
- Impairments of the upper limb (Motricity Index, Ashworth Scale);
- Functional status (Short Physical Performance Battery, Wolf Motor Function Test);
- Disability (Barthel Index);
- Depression (Geriatric Depression Scale) and Quality of life (Stroke Impact Scale).
Treatment protocol
The rehabilitation protocols used for treating the patients of the intervention group is designed according to the principles of the Carr and Shepherd “Motor relearning program”.
Patients who accept to participate in the study receive a detailed explanation of how the long term treatment works. The role of the hospital (patient education and updating treatment
plan), the importance of home practice (regularity, intensity of training) and the role of the kiosk (both continue practice and assessment by the Habilis platform). Afterward, patients
are instructed, within the hospital setting, to practice a given list of therapeutic exercises aimed at improving upper limb function by using rehabilitation devices provided by AUSL11
(different shape and size objects to manipulate, puzzles, printed paths to follow with pens of different shape and size). In addition the patient is trained to use patient Habilis platform
which he will find in the most convenient kiosk near his home.
If necessary, a caregiver may be involved in the entire process of training to instruct him/her on the best way to assist the patient, if needed.
At the end of the instructional period (3-5 2-hour training sessions in hospital) patients are given:
- all the rehabilitation devices needed for practice at home (“rehabilitation suitcase”);
- the list of the exercises to perform at home, with specification of frequency and intensity of exercise training (“home program sheet”);
- a logbook where indicate the execution of the given tasks;
- the weekly time schedule in which the kiosk will be available for him.
Patient is requested to go at the kiosk level 2-3 times a week and practice the same home exercises while assisted by the patient unit of the Habilis platform. He is instructed not to bring the “rehabilitation suitcase” since the entire set of rehabilitation devices is available in the kiosk, ready for him. From the doctor unit of the Habilis platform located in the hospital, a physiotherapist observes patients’ performance at least once a week, gives advices for improving practice and at regular intervals reassesses the patients. The patients may also request advice from the physiotherapist via Habilis platform.
Kiosks are supervised by volunteers which assure opening/closing the door of the kiosk, cleaning the environment, maintaining the equipment in proper order and ready-to-use, start emergency procedures, if needed. A caregiver may assist the patient in kiosk activities if needed.
Patients are monitored during treatment at least once a week by videoconference and results quantified by Motricity Index-upper limb.
If the treatment plan needs to be revised or in the presence of adverse clinical events the physiotherapist asks the patients to return to the hospital to review the treatment program or a visit with a MD. In the former case the same procedure stated above for patient/caregiver education are reapplied.
After 3 months patients are reassessed again at hospital level. During the final assessment also patient’s, caregiver’s and health professional satisfaction will be investigated.
Outcome assessment
Outcome parameters
Secondary endpoints will be considered those measures related to domains which may influence the outcome of rehabilitation treatment (here reported for conceptual domain).
- Demographic characteristics
- Age (years)
- Gender (male/female)
- Anthropometric characteristics
- Weight (Kg)
- Height (m)
- Body mass index
- Social characteristics
- Marital status (single/married/divorced)
- Social and family support (questionnaire)
- Educational status
- Formal education (years)
- Pre-morbid ability of computer use (no/yes)
- Home characteristics
- Floor level of the apartment
- Internal barriers (no/yes)
- External barriers (no/yes)
- Kiosk accessibility
- Home-kiosk distance (km)
- Time required to go from home to kiosk (minutes)
- Need of help to get to the kiosk (no/yes)
- Transportation needed (yes/no)
- Stroke characteristics
- Side of the motor impairments (right/left)
- Presence of contra-lateral motor impairments (no/yes)
- Neglect (no/yes)
- Associated arm impairments
- Shoulder and hand pain (Visual analog scales)
- Wolf Motor Function Test
- Spasticity (Modified Ashworth Scale)
- Sensibility disorders (no/yes)
- Co-morbidity
- Co-morbidity Severity Index of the Cumulative Illness Rating Scale (CIRS)(50)
- Mini mental state examination
- Associated neurological limitations
- Cerebellar signs
- Extrapyramidal signs
- Mobility limitations
- Short Physical Performance Battery
- Disability
- Barthel Index
- Nottingham Extended Activities of Daily Living
- Depression
- Geriatric depression scale
- Quality of life
- Stroke Impact Scale
- Adherence to treatment program
- At home (number of exercise sessions)
- At Kiosk (number of exercise sessions)
- Customers’ opinion and satisfaction (ad-hoc questionnaire)
- Hospital program
- Home practice
- Kiosk practice
- Whole rehabilitation program
- Caregivers’ opinion and satisfaction (ad-hoc questionnaire)
- Hospital program
- Home practice
- Kiosk practice
- Whole rehabilitation program
- Clinicians’ opinion and satisfaction (ad-hoc questionnaire)
- Hospital program
- Home practice
- Kiosk practice
- Whole rehabilitation program
- Safety
- Adverse clinical events (number and type)
Outcome measures
Baseline and final 3-month follow-up assessments will be carried out in hospital settings by a medical doctor and a physiotherapist. Once a month adherence to home and kiosk program will
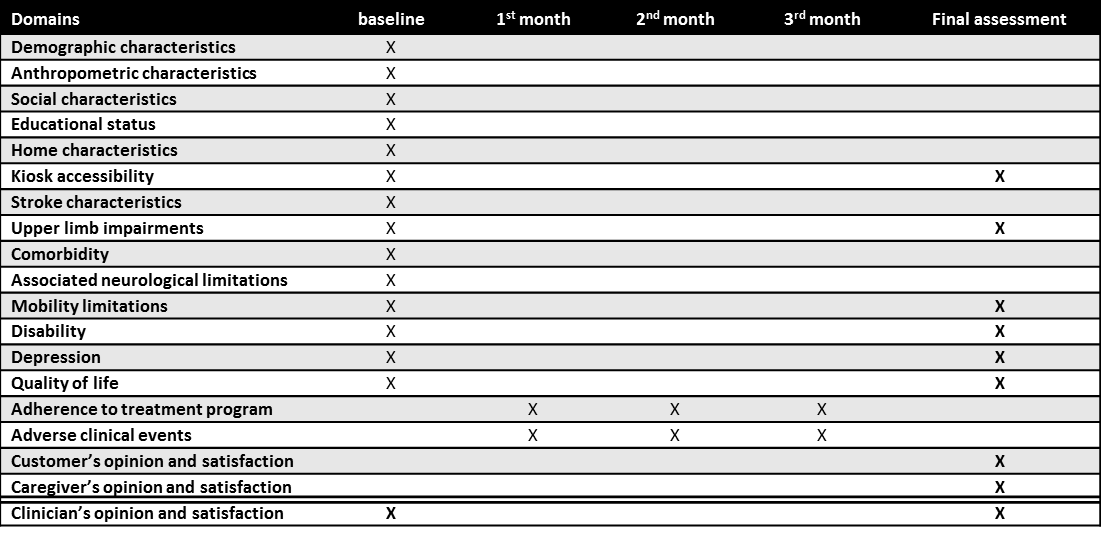
be recorded from the logbook for home practice and from Habilis platform for kiosk practice. In Table 1 the timing of recording of study parameter is summarized.
Withdrawal
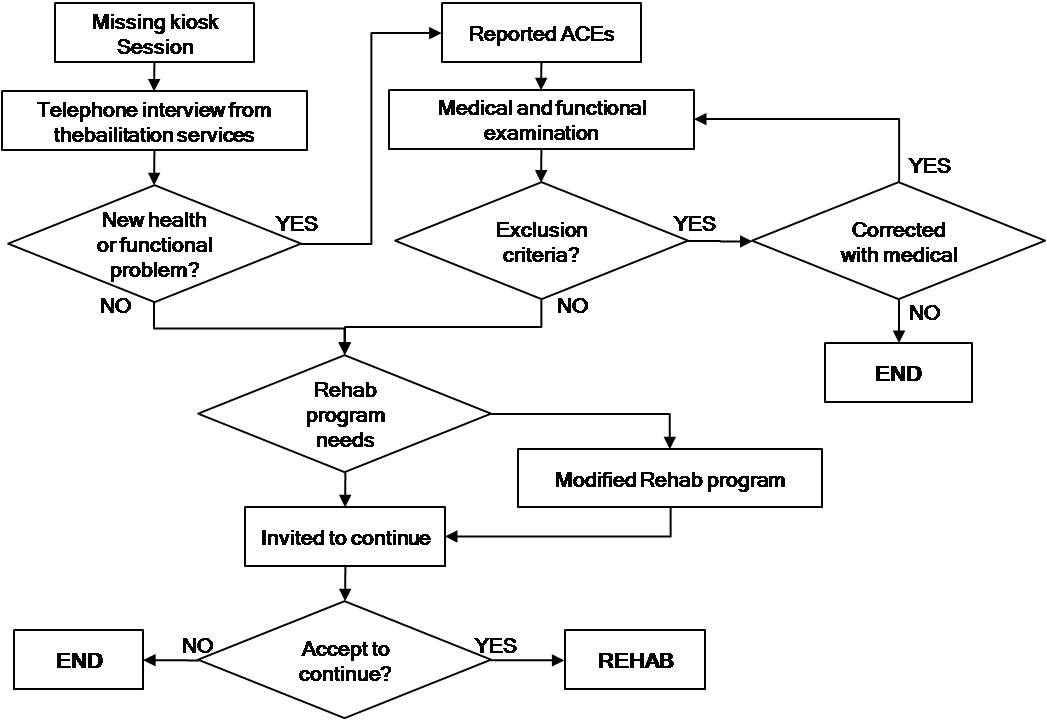
Subjects can leave the study at any time for any reason if they wish to do so without any consequences. The clinician can decide to withdraw a subject for urgent medical reasons. Subjects withdrawn from treatment will be dealt according to the procedures shown in Figure 7.
Protocol flow chart
Osteoarthritis of the hip - MUW (Medial University Warsaw) [PL]
Description of the scenario
1 - Characterization of the patient
Mrs. Danuta is 74 years old and she is retired. She suffers on hip pain due to coxarthrosis. Her pain in groin and hip and femur is deterioration leading to disabilities in her daily living. She is depressed with low self assessment concerning physical and mental health. She lives alone at home. Her son visits her twice a week and only then helps her in daily living. Mrs. Danuta is awaiting her total hip replacement. She is treated in University Clinic (Chair and Department of Orthopedics and Traumatology of Locomotor System). The waiting list requires one year for THR surgery.
2 - Description of the traditional treatment
The traditional treatment is based on two models. The one is neglecting physiotherapy model in which patients are not referred to physiotherapy prior the surgery because of potential pain exaggeration after exercises. The second model is physiotherapy is physiotherapy oriented model in which patient is focused on general endurance and fitness improvement before surgery to enhance early postoperative period. The treatment consists of individual exercises and physical therapy to alleviate pain, if applicable. The patient’s status has to be recognized to tailor the set of exercises. Treatments vary from daily through 3 times a week to 2 days per week. Patients are usually treated out patiently. The effectiveness of pre-operative physiotherapy in OA of the hip is anticipated. Accordingly to our own study the percentage of patients who took part in preoperative rehabilitation is 60%. Most of them received their exercises at home (33%), out patiently (30%), in organized form in sanatorium (18%) or in patiently in rehabilitation clinics (15%). The rest attended other forms of rehabilitation (4%). The main effects gained after physiotherapy in hip OA consisted of pain relief and improve or maintain muscle function and joint motion.
3 - Patient Recruitment
The medical evaluation of Mrs. Danuta by orthopaedic surgeon leads to conclusion that referring her to physiotherapy should improve her affected extremity prior to her surgery and prepare her to post surgery period. She should gain also better endurance and improve function of whole her musculoskeletal system. Mrs. Danuta should improve the strength of her muscles and increase the Range of Motion in her affected extremity using Habilis Platform. Having the Habilis Platform at home she can exercise without unnecessary travel to the outpatient clinic or elsewhere, being supervised on demand or even permanently by her physiotherapist and/or orthopaedic surgeon on remote.
4 - Description of the tele-rehabilitation program or the tele-care for the patient
The exercises provided by the CLEAR project system are delivered for 4 weeks. The patient receives detailed instructions and supervised hands on training in the Clinic by the therapists. Mrs. Danuta receives full information how to log in the CLEAR system with her personal code and how use the Habilis platform. The telerehabilitation unit consists of the computer with web cam and headphones supplied with the Internet access and some rehabilitation tools like rubber tension band, weights for exercises, step, etc. The set is delivered to the patient’s home by Local Service Provider. The computer is equipped with the touch screen for ease the usefulness of the system dedicated to be used by unskilled people. Mrs. Danuta performs selected exercises tailored for her considering her general and local health. The set of exercises is individually tailored by selection out of the pool of the exercises. The individual program should help the patient to prepare for total hip replacement (THR) procedure. There are some exercises related to range of motion (ROM) optimization of the hip joint as well to strengthen hip muscles. Breathing exercises, upper extremity and trunk exercises are elaborated to supplement local ones. The patient is also advised to participate “her rehabilitative training” 5 times a week, about 60 minutes per session. Utilizing the Habilis Platform and the CLEAR system the patient can log in to it and use prepared for him/her video clips. The short movies instruct the patient how to perform exercises. The therapist selects exercises for particular patient like Mrs. Danuta out of an archive database ready to perform. The average daily set of exercises consists of nine exercises (including breathing exercises).The patient uses a webcam tele-consultation with a physiotherapist once a week and orthopaedic supervised remotely session if required. Having the on line supervised videoconference session; the physiotherapist is able to point out well and ill performed exercises and reminds some restrictions if required and instruct directly what should be improved. The physiotherapist can give the feedback about training schedule or performed exercises.
5 - Description of a tele-reabilitation session
Patient logs on to the system using individual account user name and password. The platform automatically responds with personalized message that indicates the sort and number of exercises to execute. Mrs.Danuta has assigned an individual set of exercises tailored for her individually. She executes them at the particular day of her telerehabilitation program. Patient may watch the tutorial how to perform and to know what equipment should be used if any. Patient is obliged to record an example how the exercise is performed using the webcam and recording options. The patient can add some comments for the therapist.
6 - Description of the interaction with the therapist
The patient is examined during a clinical consultation before beginning home therapy exercises. The examination includes joints range of motion, muscle strength and lower extremities measurements. Patient fills up several questionnaires specific for musculoskeletal disorder i.e. Harris Hip Score (HHS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Hip disability and Osteoarthritis Outcome Score (HOOS) and general quality of life instruments like Short Form – 36 (SF–36) and Visual Analogue Pain Scale (VAS). The patient’s condition and quality of life is evaluated similar way during follow up after telerehabilitation program. Personal physiotherapist contacts the patient during telerehabilitation period give the feedback focused on individual training program. Every week Mrs. Danuta is contacted by her personal therapist. The therapist is able to rearrange exercises or tailor them again considering the progress made by the patient. Additionally, personal physiotherapist can invite the patient again to the Clinic for personal “face to face” checkup.
7 - Description of the therapist session
Each therapist connects to the platform daily. The system automatically shows whether recorded exercises are stored by patients for evaluation. There is also visible information how patient comply and adhere to assigned therapy program. For example the therapist can contact Mrs. Danuta to give her feedback about her training and give her individual advices, including the need of the therapy rearrangement and tailoring a new therapy. The therapists can display the exercises at high speed, and score them. Subsequently the scores serve for evaluation the progress of the therapy.
8 - Description of the advantages the programs has for the patients
In particular example Mrs. Danuta feels happy and satisfied with her everyday exercise program moving nowhere from her home. She lives far away from the Clinic so her daily journeys to attend rehabilitation program at the outpatient clinic would fatigue her very much. Saving the transportation costs with telerehabilitation is very important for her as well. She observes advantages and her personal improvements whit her rehabilitation program progress. She is sure there is her physiotherapist and her doctor just behind the computer screen and she feels safer than being alone without the platform. She is sure that she has good and professional rehabilitation care. Mrs. Danuta feels happy because rehabilitation made with the Habilis platform is not boring and at the same time she gains new skills how to use the computer. She concludes that telerehabilitation enables patients to do exercises in their natural environment - at home. Patients do the exercises for 4 weeks remotely mentored by therapists. This is considered as a huge motivation for patients. The huge advantage is also that the patient can do exercises without certain time limits like Outpatient Clinic working hours and the schedule.
9 - Description of the advantages this program has for the therapist
In short word this program has for the therapists several advantages including saving time and money for approach to patients, making the working time more adjustable and flexible. Supervised remotely rehabilitation has the documentation better and well defined. Recorded clips sequence shows perfectly the progress being made by the patient. This particular solution opens a huge opportunity for the physiotherapist to work at home that may be particularly advantageous for disabled or for those who must remain at home.
10 - List of the participants at the definition of the scenario
| Name participat | Profession | Company | Contact e-mail |
|---|---|---|---|
| Anna Kostrubala | Physiotherapist | MUW | telerehabilitacja@gmail.com |
| Karolina Krawczak | Physiotherapist | MUW | telerehabilitacja@gmail.com |
| Dominika Cabaj | Physiotherapist | MUW | telerehabilitacja@gmail.com |
| Wojciech Glinkowski | Orthopaedic Surgeon | MUW | telerehabilitacja@gmail.com |
Clinical Protocol
Here below the protocol on hip and knee osteoarthritis rehabilitation designed by MUW (Medical University of Warsaw) is described.
Overview
The hip and knee osteoarthritis patient with severe and chronic joint pain are treated at Orthopaedic and Traumatology Clinic either conservatively or surgically.
Surgical approach covers mostly total hip replacements (THR) and total knee replacements (TKR). Patients are assessed and put on the waiting list due to National
Health Care Fund requirements. In some cases the waiting time may take more than 12-18 months. National Health Care System allows to provide rehabilitation prior
the surgery however an access to rehabilitation is similarly regalement. That means the patient need to await the therapy. Disabilities of the patients located in
most important joints of the lower extremity lead to decrease of locomotion abilities that additionally lower the attendance to rehabilitation process prior surgery.
Moreover, the same referral system leading to waiting lists acts postoperatively so that additionally diminishes an attendance to postoperative rehabilitation. The most
of the literature search confirms that pre hospital teaching as well physiotherapy may reduce in-hospital anxiety, improve coping and rehabilitation compliance during
hospital stays of surgical patients. Patients who had received rehabilitation therapy and teaching are less anxious at the time of hospital admission and at discharge,
and also more likely to have practiced physiotherapy exercises. Positive attitude as well exercises decrease significantly rehabilitation and occupational therapy and
physiotherapy while in hospital, and after the discharge. It can be anticipated that whole educational and mostly tele-rehabilitation program may further improve outcomes.
The implementation of the Habilis service will be placed as an added value to the outpatient rehabilitation of the preoperative and postoperative cases treated on home
based rehabilitation. The implementation of tested tele-rehabilitation service shall diminish total therapy costs, empower patients, supervise and motivate patients to
attend rehabilitation on daily base at home. Tele-rehabilitation service implementation in preoperative period may prepare and activate patient to shorter hospital stay
earlier return to supported locomotion that may influence on overall postoperative complications rate. Introduction of tele-rehabilitation is going to increase the availability
of rehabilitation service by crossing over distances and environmental and atmospheric obstacles. Surveyed patients in Clinical Centre clearly pointed out the influence of
atmospheric conditions on their willingness to attend tele-rehabilitation treatment at home. Tele-rehabilitation objectives improve monitoring of recovery progress that leads
to Evidence Based Rehabilitation by utilizing IT enhanced tools and data warehousing and analysis. Many patients disabled by hip or knee osteoarthritis are still active in their
professional activities that may allow them to return to professional activities earlier, having their rehabilitation ongoing. The CLEAR tele-rehabilitation approach is aimed to
improve the physical function by individually adjusted exercises related to muscle strength training, coordination, and proprioceptive control. Simultaneous and/or consecutive
online service by remote physiotherapist and supervising orthopaedic surgeon during tele-rehabilitation service is the additional advantage of CLEAR approach.
Target Patient Group
Population (base)
Participants receiving an outpatient rehabilitation program prior and after Total Joint Replacement due to osteoarthrosis of the hip and knee joints (chronic disease that affects seriously elderly population).
Inclusion criteria
The inclusion criteria are:
- capability to participate following outpatient treatment (3 days per week minimum);
- motivated;
- fluent in National language (or English);
- 35 Years and older;
- Admitted to Department Orthopaedics and Traumatology of Locomotor System and/or its outpatient clinic;
- Primary impairment diagnosis of osteoarthrosis of the hip or knee joint;
- Clinically and radiologically confirmed diagnosis;
- Awaiting Total Hip or Total Knee Replacement or just already operated patient.
Exclusion criteria
The exclusion criteria are:
- unable to provide informed consent due to dementia and severe persistent delirium;
- inability to cooperate with the clinical protocol;
- cardiac or other medical instability that would preclude carrying out high intensity exercises;
- insufficient understanding of the National or English language;
- visual, or hearing barriers to participation;
- presence of currently ongoing musculoskeletal injuries except unilateral proximal femur fractures that requires Total Hip Replacement;
- presence of metastatic cancer, including cancer that causes a pathological fracture;
- lifetime psychosis or mania;
- alcohol or substance dependence within 6 months, or current alcohol or substance abuse;
- age <18 years.
Admission and baseline assessment
Each osteoarthritis patient is referred by his general practitioner (GP) to orthopaedic surgeon at the Clinic Centre and later qualified to THR or TKR surgery. Patients name
is located on waiting list. Typically patients are invited for a surgery with invitation letter that contains concise orthopaedic advices for preoperative period. Preoperative
rehabilitation can be prescribed by supervising general practitioner but that is rather rare. After admission to orthopaedic department and after surgery patient is taught how
to manage his/her new hip or knee. At admission patient is interviewed and examined. Preoperative questionnaires are utilized for further investigation and assessment. Tests
include physical examination, measurements as well self assessment quality of life type questionnaires. After discharge patient is referred in reasonable time to rehabilitation
outpatient clinic that requires another waiting list to be consulted by rehabilitation specialist than therapy is determined. Such procedure that follows the health care system
regulations prolongs. Any further therapy is considered after rehabilitation physician consultation as well in referral model.
Postoperative rehabilitation protocol is designed for direct postoperative patients as well for patients discharged already from the Clinical Centre. The traditional way consists of
movement restrictions and weight bearing precautions with introduction to postoperatively recommended exercises and behaviours. The Habilis service for orthopaedic cases is the novel
approach that supplements simple procedures traditionally implemented. The CLEAR service plan is based on the same postoperative protocol that patient receives at the discharge from
the hospital. Daily exercises are prescribed on the same base. However, it is expected that attendance to their execution at home may differ if patient keeps tight contact with
his/her physiotherapist via tele-rehabilitation or not.
Treatment protocol
The added value of the home-based exercise program is a technology that supports physiotherapy intervention for patients with chronic musculoskeletal disorders. The program is facilitated
with notebook pc with new developed software giving access to a database of exercises. The treatment progress is documented by the patients who record his/her performance of selected
exercises to be assessed by the therapist off line. Patient and professional are able to contact each other by internet based videoconference, incorporated into the system. Chat, email
or phone contacts are available in any urgencies. Supplemental vital monitoring devices can be applied in cases that require more detailed monitoring. Otherwise the physiotherapist and/or
physician connect the patient once a week, at a fixed time. Questions asked by patient are answered during patient-therapist connection. Automatic survey is provided timely while shutting
down the PT session and data (charts and video) are recorded. Details of exercise program modifications are recorder too. Exercises can be added or removed from the tailored exercise
program for the particular patient.
Subjects will receive the telerehabilitation program supervised remotely. The home base exercise program will consist of scheduled, osteoarthritis oriented designed rehabilitation program.
An application for telerehabilitation service is supplemented with a database of exercises and various communication modalities (email, chat, and video-conference) for patient
– professional interaction. The Clinical Centre will provide home based exercise program for most frequent chronic musculoskeletal disorders – osteoarthritis of hip and knee that
require Total Joint Replacement. During the outpatient visit the patient will be trained to maintain and operate application and hardware and also to participate the program.
Similarly the post-surgery group will have the training during their hospital stay after the surgery. Home based program training for this group will take place in the hospital
before discharge. Prior the surgery for preoperative group and pre- and postoperative groups notebook PC will be installed at the patient’s home by Lo.S.P. employee. After this period
home based rehabilitation program will be executed and continuously provided until its end after 4th week of the program. Physiotherapists will be available for remote contacts with
patients (and on site if necessary) at the clinic during scheduled time.
The set of selected and required exercises for the patient will appear in the scheduled rehabilitation individual settings. Precautions and warnings reminder will appear regularly as
an entire part of rehabilitation program. The application provided through the Habilis platform gives the patient an opportunity to schedule the exercise program throughout the whole week.
After the treatment program a follow-up day is scheduled. The main study parameters are compliance with the home based exercise program, satisfaction regarding the home based exercise
program, clinical effect outcomes and economical benefits of the home based exercise program. Assessed clinical status is based on outcomes protocols accepted worldwide.
During the stay in the Centre
Patient from preoperative group is invited 2 month prior the planned surgery and trained in the facility how to play with the Habilis platform (notebook, webcam, other equipment i.e. Therabands) Separate training room is prepared for that purpose. Two tutorial and practical testing meetings are planned on site. Additional meeting is possible if required. During the meeting younger and more cooperative family member can be actively present to learn how to cope with the Habilis platform. The letter with information with instructions describing proper way of preoperative period home "self-training" will be send to other patients who are not selected for the TR Service. Postoperative group of patients is trained postoperatively during postoperative hospital stay. Hospital stay may take from few days up to two weeks until "stiches" are removed from the wound. Usually in minimally invasive surgery the hospital stay is shorter. In standard surgical approach the hospital stay can be a little longer. Informed consent for patients-participants is undersigned.
Remotely
Patient is supplied with the Habilis platform by Lo.S.P. The provider is responsible for proper installation of the TR service components for patient use. Tests are performed
right after installation. Equipment security measures are ensured, including free rental agreement, insurance signature per patient personally is preferred assurance method.
More often contact with physiotherapist as well with orthopaedic surgeon can be considered as an advantage for patient’s participation. Payment for patient’s participation in
the study is not considered as a method of patient’s recruitment.
The Lower rate of complications for TR service patients and better opportunities for more frequent contact with orthopaedic surgeon should be a motivation for TR patient to
participate. Supplemental monitoring utilized in selected cases may improve additionally overall safety of tele-home care.
Outcome assessment
Outcome parameters
This protocol shall examine the course of pain and physical function as measured by the condition-specific patient questionnaires [including the Western Ontario and McMaster Universities
Osteoarthritis Index (WOMAC), the generic health status measure, Short Form-36 (SF-36)] and other assessment instruments. This clinical protocols that include inclusion criteria,
exclusion criteria, preadmission clinical status, post therapy status and short time follow up. Clinical status is based on outcomes protocols accepted worldwide: SF-36, WOMAC,
Harris Hip score, ROM, VAS, HOOS, KOOS, and other hip and knee instruments. The most commonly used outcomes were function, predominantly subjective measures of functional ability,
and range of joint motion as an objective measure. While range of joint motion is important, its usefulness as an outcome measure of physiotherapy interventions is limited as other
factors, such as prosthetic design, preoperative knee motion, and surgical technique, also influence postoperative range of joint motion.
Pain intensity and fatigue will be assessed with VAS scales. The VAS consists of a 10 cm horizontal line with ‘no discomfort at all’ on one end of the scale and ‘as much discomfort
as possible’ on the other end of the measure line.
Disability will be evaluated utilizing worldwide known and accepted assessment instruments (Merle d’Aubigneu Score, Harris Hip Score, HOOS, Knee score, KOOS, WOMAC, Oswestry Disability
Score). Neuromuscular assessment will be supported with isokinetic testing device. Modification of walk test for musculoskeletal purposes can be used as supplementary measure.
Hand grip strength dynamometry may be applicable in osteoporosis-osteoarthrosis cases. The measurement will follow proper methodology of testing. ROM test as an assessment
instrument is an inter- and intra examiner reliable instrument. It measures the range of movement in many axes - flexion/extension, abduction/adduction and rotation movements that
can be performed by joints in active and passive mode. Videoconference assisted method of ROM assessment for remote assessment and instrumental measurement will be provided to
assess the Range of Movement progress.
Back postural assessment with kyphosis and lordosis angles will be measured utilizing dedicated structural light method with Debrunner’s type of assessment methodology.
Isokinetics of lower extremities will be assessed with Smart Box Lift device and dedicated software (Humac Norm, USA).
The economics will be assessed by comparison of time and resources consumption for treatment modalities (telerehab. vs. traditional rehab approach including cost and time of travel).
The main outcome parameter are therefore:
- SF-36: a multi-purpose, short-form health survey with only 36 questions. It yields an 8-scale profile of functional health and well-being scores as well as psychometrically-based physical and mental health summary measures and a preference-based health utility index. It is a generic measure, as opposed to one that targets a specific age, disease, or treatment group. Accordingly, the SF-36 has proven useful in surveys of general and specific populations, comparing the relative burden of diseases, and in differentiating the health benefits produced by a wide range of different treatments.
- WOMAC: a set of standardized questionnaires used to evaluate the condition of osteoarthritis patients. The Index is self-administered and assesses the three dimensions of pain, disability and joint stiffness in knee and hip osteoarthritis using a battery of 24 questions.
- ROM scale: to be used as an evaluative instrument in rheumatoid arthritis (RA) trials. The EPM-ROM Scale evaluates 10 distinct movements of the small and large joints. The score of each joint varies from 0 (full movement) to 3 (severe limitation) and the cut-off degrees of motion are, in general, based on the lack of ability to perform some determined activities of daily living.
- HOOS: The Hip disability and Osteoarthritis Outcome Score (HOOS) is developed as an instrument to assess the patient’s opinion about their hip and associated problems. Is intended for use in hip disability with or without hip osteoarthritis. Can be used over short or long time intervals; to assess changes from week to week induced by treatment (medication, operation, physical therapy) or over years or to describe populations. HOOS consists of 39 items, in 5 sub-scales; Pain (P) – nine items, Symptoms other, including stiffness (S) – five items, Activity limitations, daily living (A) – seventeen items, Activity limitations, recreation and sport (SP) – four items, and hip-related Quality of life (Q) – four items.
- KOOS: The Knee injury and Osteoarthritis Outcome Score (KOOS) was developed as an extension of the WOMAC Osteoarthritis Index with the purpose of evaluating short-term and long-term symptoms and function in subjects with knee injury and osteoarthritis. The KOOS holds five separately scored subscales: Pain, other Symptoms, Function in daily living (ADL), Function in Sport and Recreation (Sport/Rec), and knee-related Quality of Life (QOL). The KOOS has been validated for several orthopaedic interventions such as anterior cruciate ligament reconstruction, meniscectomy and total knee replacement. In addition the instrument has been used to evaluate physical therapy, nutritional supplementation and glucosamine supplementation. The KOOS is a valid, reliable and responsive self-administered instrument that can be used for short-term and long-term follow-up of several types of knee injury including osteoarthritis. The measure is relatively new and further use of the instrument will add knowledge and suggest areas that need to be further explored and improved.
- Harris Hip Score: accorded five points to the mobility dimension that could under certain circumstances rate an arthrodesis above an arthroplasty. This scale conspires from 3 sections: 1st section serves to value: pain, support, distance walked, stairs, sitting, activities - shoes, socks, sitting and public transport, 2nd about patients range of motion and 3th, the last one, about total degrees of flexion, abduction, adduction and external rotation.
- End-users (both patients and professionals) satisfaction with the computer enhanced, home based, remotely supervised exercise program;
- Usability of the tested program;
- Outcomes improvement of the computer enhanced, home based, remotely supervised exercise program;
- Patient's compliance assessment.
Outcome measures
The clinical assessment will be provided immediately after enrolment prior to home based exercises. Weekly remote assessment will consist of questionnaires and remote assessment. Immediately after home based exercises period, one month and 3 months after home based exercises intervention examination a follow-up day is scheduled. The main study parameters are compliance with the home based exercise program, satisfaction regarding the home based exercise program, clinical effect outcomes and economical benefits of the home based exercise program. Assessed clinical status is based on outcomes protocols accepted worldwide.
Withdrawal
Subjects can leave the study at any time for any reason if they wish to do so without any consequences. The clinician can decide to withdraw a subject for urgent medical reasons.
Protocol flow chart
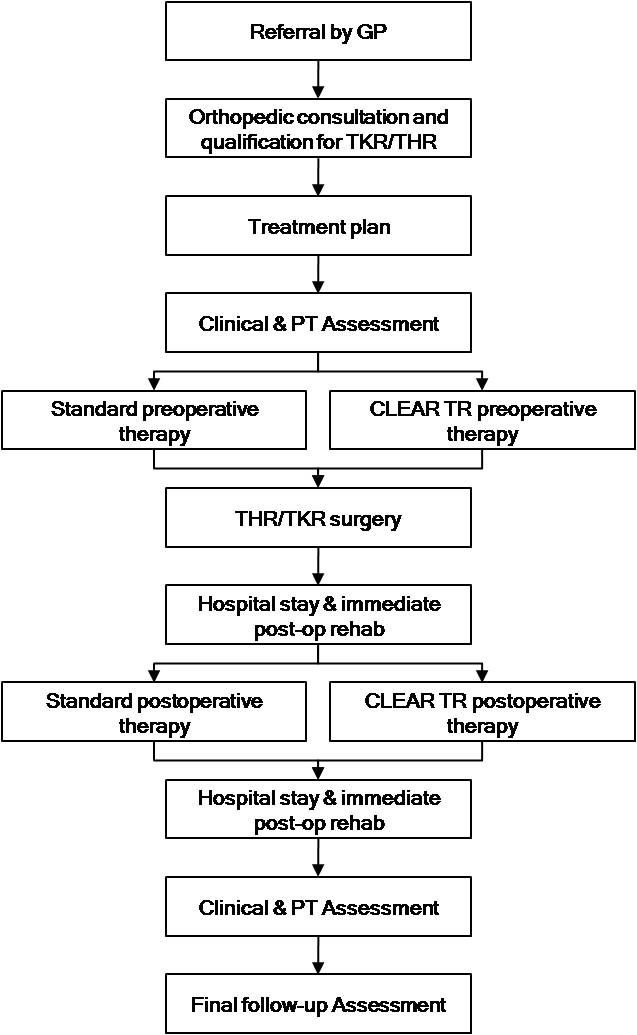
Non-specific pain - RCR (Stichting Revalidatiecentrum Het Roessingh) [NL]
Description of the scenario
1 - Characterization of the patient
Margret is 29 years old. She is working at an administration department and predominantly performs computer work. Margret suffers from pain in her lower back. Because of the pain she had to reduce the number of working hours and she even did quit here dancing lessons. She danced 3 times a week and enjoyed it very much. Now she is anxious to move. She thinks every movement leads to pain and will damage her back. Because of these ‘cognitions’ she doesn’t exercise anymore, she even avoids social activities because she believes these might cause damage to her lower back also. As a consequence, she ended up in a vicious circle of avoidance and pain. Margret’s husband attended her on her pain-related behaviour and advised her to seek help.
2 - Description of the traditional treatment
Therefore, Margret decided to go to her general practitioner (GP). Her GP referred her to ‘Roessingh Centre for Rehabilitation’, a rehabilitation centre in the east part of the Netherlands. Het Roessingh has been officially acknowledged as an ‘innovation centre for pain rehabilitation’ by the Dutch government. Margret was invited for the intake with the rehabilitation physician. Thereafter, an additional intake was conducted by the physiotherapist and social worker. Due to the fact that Margret reported a high score on kinesiophobia, a psychologist was included in the rehabilitation. Three weeks after the intake, Margret started a cognitive-behavioural treatment programme. This treatment in the rehabilitation centre is performed in a group with other lower back pain patients (maximum of 6 persons). The total duration of the rehabilitation programme is 8 weeks. Thanks to the cognitive-behavioural treatment approach, Margret is being treated by a different of disciplines (e.g. rehabilitation physician, occupational therapist, vocational therapist, physiotherapy, sports therapists and psychologist).
3 - Patient Recruitment
During the first two weeks of the treatment, Margret visits the rehabilitation centre three times a week, for half a day each, to get insight in her maladaptive cognitions and pain-related behaviour. In addition, Margret is taught how to cope with her pain. During the first two weeks the physiotherapist explains Margret how to exercise most optimally and, in parallel, how to use the CLEAR system. The CLEAR treatment facilitates the transfer of the skills she learned in the clinic to her daily life. During the last 6 weeks of the treatment programme, part of the intramural physiotherapy and sports therapy lessons can be replaced by the CLEAR tele-rehabilitation session at home. Margret can choose from the exercises which are set by the physical therapist.
4 - Description of the tele-rehabilitation program or the tele-care for the patient
Once at home, Margret has to visit the CLEAR website. After logging in with her personal code, she is able to view her weekly exercise programme. er exercise programme consists of a selection of videoclips together with a verbal and textual instruction(s) of the physical exercises the therapist selected for her. Margret started with a basic set of exercises aimed at improving force, mobility, coordination, and condition of her lower back. Her therapist requested her to record one of these exercises. This exercise will be available on the website for the therapist. This recording can be used by the therapist to ‘monitor’ the progress of Margret’s treatment over the weeks. In addition, Margret is able to add a short text message ( ‘patient comment’ ) to the therapist about possible questions or difficulties she perceived while training. Once a week a videoconference will be set up with the therapist according to schedule (on a fixed time of the week, Margret has a videoconferencing with her therapist).
5 - Description of a tele-reabilitation session
Under the supervision of the therapist, Margret started with the execution of a tailored set of exercises to reduce her kinesiophobia. While executing, the therapist provided Margret feedback on her performance. This feedback is important for Margret since it gives her a feeling of safety and confidence. Together the therapist and Margret discuss the way she executed the exercises and what she felt.
6 - Description of the interaction with the therapist
A webcam is incorporated in the system, so the exercises can be recorded by the CLEAR system and discussed with the physical therapist by means of videoconference. Feedback will be given on performance (motivational feedback, feedback on the quality of the exercise) and questions from the patient. Therefore an appointment is made for ten minutes once a week.
7 - Description of the therapist session
The therapist connects to the platform and examines the performances of the patient in the previous sessions. He or she assigns exercises for the next week related to the results obtained so far. During the ten minute appointment with the patient the therapist logs into the system and talks to the patient by means of videoconference.
8 - Description of the advantages the programs has for the patients
Thanks to this remote treatment, the patient has had the opportunity to continue seeking a personalized and individualized therapy schedule by a therapist tailoring the treatment to their specific deficits without having to afford transportation or wasting time traveling to the rehabilitation centre.
9 - Description of the advantages this program has for the therapist
The therapist can establish an individualized treatment for the patient, saving time and money. The therapist has also the opportunity to discuss things individually with each patient. In the traditional program this isn’t possible.
Clinical Protocol
Here below the protocol on chronic pain designed by RCR (Rehabilitation Centre Het Roessingh) is described.
Overview
The pain of patient with chronic pain can be located in different body areas (e.g. neck/shoulder, lower back, multiple points) and can have different causes varying from very
specific like being a result of a trauma or nonspecific which is most often the case. Chronic pain is considered to be multifactorial. Physical, psychological and social factors
are important. A lot of patients with chronic pain develop a deconditioning syndrome (Mayer et al., 1985) little by little the patient becomes less active both physically and
socially. As a result of pain, patients avoid being active, their physical condition decreases with the consequence of more pain when performing the same or even less physical
exercises. Patients can become depressed or develop passive coping strategies like catastrophic ideas of pain and anxiety emotions due to a delayed recovery. Most chronic pain
patients complain about sleep disturbance, in the morning they awake tired, stiff and with pain. In daytime these patients become irritated, which results in more decrease in
physical activity and physical condition (Akkerveeken et al., 1992).
The patients with chronic pain can be patients with chronic (lower) back pain, chronic neck/shoulder pain, fatigue problems (like chronic fatigue syndrome), whiplash problems
and complex pain problems. “Whiplash is an acceleration-deceleration mechanism of energy transfer to the neck. It may result from rear-end or side-impact motor vehicle collisions,
but can also occur during diving or other mishaps. The impact may result in bony or soft-tissue injuries (whiplash injury), which in turn may lead to a variety of clinical
manifestations (whiplash-associated disorders)” (Spitzer, 1995). In 20 to 30 percent of all whiplash cases chronic pain develops (richtlijnen whiplash, 2008). Patients with
a whiplash are classified to Whiplash associated disorder (WAD) grade 1 and 2. The average WAD pain patient belongs to the lower socio-economic class, they are less satisfied
with their work situation and they have an extern locus of control.
In every socio-economic class there are patients with low back pain. In various professions there is a higher risk of developing low back pain. Especially professions where
workers are exposed to (heavy) physical work (Burdorf et al., 2002). The cause of low back pain is often multi-factorial. Most CLBP patients develop a deconditioning syndrome
as described above characterized by fear of moving resulting from the fear of pain with the consequence that they become less active and their physical condition decreases (Mayer
et al., 1985).
The Habilis service will partly replace the outpatient rehabilitation of the chronic pain rehabilitation group treatment by home training. The rationales for doing this are
multiple: it will contribute to a reduction of costs; it enables patients to more easily translate the learned skills to every day life; it fits in the current trend of self
management of the patient and it enables patients to exercise much more at moments preferred by the patient and as such makes treatment at least as or even more effective.
To get insight in whether these aims are being fulfilled each individual patient is monitored on time needed by professionals in the new way of care provision and by changes
in health outcome achieved during treatment with the Habilis service as partly replacement of traditional care.
Target Patient Group
Population (base)
Participants receiving an outpatient rehabilitation program and suffer from chronic pain; chronic low back pain (CLBP) or Whiplash Associated Disease (WAD).
Inclusion criteria
The inclusion criteria are:
- chronic non-specific pain (> 3 months);
- motivated;
- capable of following outpatient treatment;
- a psychoneurotic score (SCL) lower than 150 point (symptom checklist (SCL-90));
- control of the National language;
- age >18 years old.
Exclusion criteria
The exclusion criteria are:
- insufficient understanding of the National language;
- iBMI > 35;
- age <18 years.
Admission and baseline assessment
Every pain patient that is referred by his general practitioner (GP) or medical specialist to the clinical centre comes for a central pain intake. At first the chronic pain patient
visits the rehabilitation physician for a consultation. After this consultation the patient is asked to complete two questionnaires; the symptom check list (SCL) and the multidimensional
pain inventory (MPI). The scores on these questionnaires determine whether the patient follow inpatient or outpatient treatment. Based on the consultation and the assessment the
rehabilitation physician judges if it is necessary to schedule an additional pain intake with a social worker, psychologist, physical therapist or occupational therapist.
Additional to the general pain intake, patients with chronic pain due to lower back complaints are asked to complete two extra questionnaires: Roland and TAMPA. Tampa is a
uestionnaire about kinesiofobia and the Roland Disability Questionnaire is measuring activities of daily life. These patients also undergo a back dynamometry measurement by the
physical therapist. Those additional assessments are repeated at the end of the treatment. Based on all information about the chronic pain patient the multidisciplinary meeting decides
whether or not the patient can participate in the RRP and the treatment plan is written. In two weeks the patient is informed about this decision, the treatment plan and the RRP by an
information folder. At the start of the RRP the general physical condition of every participant is measured. Patients with WAD are asked to additional complete the COPM questionnaire.
The Canadian Occupational Performance Measure is an individualized outcome measure designed for use by occupational therapists. The measure is designed to detect change in a client's
self-perception of occupational performance over time.
The selection for the Habilis service is identical to the selection described above. All patients included to the outpatient pain rehabilitation program will also participate in the
Habilis service as such the inclusion criteria and admission procedure are the same. Patients who get information from the site or elsewhere and are interested in the Habilis service
can involve in the program by following the same procedure as described above.
The baseline measurement coincides with the intake of the rehabilitation program.
Treatment protocol
The computer supported exercise program is a home based exercise program supported by technology for patients with a chronic disease. The computer supported exercise program consist
of a tablet pc with webcam and with new developed software giving access to a database of exercises and different communication tools (like a webcam) to facilitate contact between the
patient and professional. With the computer supported exercise program the therapist composes a tailored home based exercise program for his patient. The patient can execute the program
on a self-scheduled time. Every week the patient records 2 or 3 exercises with the webcam to be assessed by the therapist. Patient and professional can contact each other by email, chat,
phone or tele-conference (with the webcam). The therapist monitors the patient and once a week, at a fixed time, he will contact the patient by one of the modalities to answer possible
questions of the patient about the tailored exercise program and to review the recorded exercises. The therapist can add and delete exercises on the exercise program of the patient
during the rehabilitation.
Subjects will receive the rehabilitation program extended with the computer supported exercise program. During eight to twelve weeks the patient visits the rehabilitation centre two
or three times a week to participate in different therapies; physical therapy, condition training and sports, occupational therapy and swimming. The computer supported exercise program
consist of a tele treatment service with a database of exercises video files and offers different modalities (email, chat, and video-conference) to allow for contact between patient and
professional. This telemedicine application is an opportunity for the patient to train at home supervised and monitored by his therapist to increase his physical condition.
The computer supported exercise program will be implemented in the rehabilitation program for chronic pain patients (CLBP and WAD) in two different ways:
- Partial replacement of the traditional rehabilitation program: within the 3-days rehabilitation program (CLBP patients) the application will be used as a replacement of 1 day treatment at the clinic. During the first part of the rehabilitation (first 2-4 weeks) the patients will visit the clinic 3 days a week to receive their rehabilitation program. They will also be trained in using the computer supported exercise program. During this period a tablet PC will be installed at the patients’ home. After this period the patient visits 2 days per week the clinic to receive his rehabilitation program and execute his tailored exercise program at home till the end of the rehabilitation program. The therapist is available for contact during the two days at the clinic and a scheduled time on the replaced day.
- Complementary to the traditional rehabilitation program: within the 2-days rehabilitation program (WAD patients) the application will be used as complement to the 2 days treatment at the clinic. During the first part of the rehabilitation (first 2-4 weeks) the patients will come 2 days to the clinic to receive their rehabilitation program. They will also be trained in using the computer supported exercise program. During this period a tablet PC will be installed at the patient home. After this period the patient remains to come 2 days to the clinic to receive their rehabilitation program and will execute their tailored exercise program at home until the end of the rehabilitation program. The therapist is available for contact during the two days at the clinic at scheduled times within the week.
The agenda function provided through the Habilis platform gives the patient the opportunity to schedule the exercise program through the week. In addition patients have the opportunity to view the exercises on their tablet pc by playing the video-files. Every week the patient records 2 or 3 exercises with the webcam to be assessed by the therapist. Also the patients are offered an email, chat and tele-consulting function (with the webcam) on the tablet pc from which they can contact their therapist in case they have questions about their exercises. Patients can support their questions with a video of their execution of the exercise. Once a week, at a fixed time, the therapist will contact the patient by one of these modalities and give the patient feedback about the compliance to the exercise schedule and the exercise performance.
During the stay in the Centre
Every patient in the RRP and the Whiplash program is included to the Habilis service and signs a paper that they will participate in the program with optimal motivation. If the patient does not comply with the exercise program the treatment will be ended prematurely. During the first 2 weeks of the program the patient visits the rehabilitation centre 3 times a week. During these 2 weeks the patient is introduced to the principles of the multidisciplinary rehabilitation program. The multidisciplinary character of the treatment implies the involvement of a wide variety of therapists. In the first and second week of the RRP 2 physical therapy sessions of both 2 hours are scheduled. During these sessions two physical therapists are present. One of the physical therapist teaches half of the group (3 patients) to work with the Habilis service. Every patient gets about 30 minutes explanation about the Habilis platform in week 1 and 2 by one of the two physical therapists. The patients also receive a detailed user manual of the Habilis service. The persons get more motivated by education/explanation of the purpose of e-treatment. This user manual explains how to use the Habilis service at home and how to create an own treatment program.
Remotely
In the remaining six weeks the patient exercises at home with HABILIS. Of the weekly 4.5 hours physical therapies and sport therapy 2 hour will be replaced by home training. The
patient visits the rehabilitation centre in those weeks two times a week to follow the program. The HABILIS service provides the patient with a standard program for increasing
strength, coordination, mobility and general condition. On top, the physical therapist creates for every patient an individual treatment plan based on individual complaints and
outcome of the general physical fitness measurement. For this individual treatment the physical therapist selects special exercises, this selection of exercise can be changed
every week by the physical therapist based on the progress / performance of the patient. Together with the psychical therapist the patient makes a schedule on when, where, how
often and what he will practice. The patient has to use the HABILIS service for exercise at least 4 hours a week. A webcam is incorporated in the system, so the therapist can
see how the patient performs the exercises at home. The patient and the physical therapies can contact each other by using the webcam for tele-consultation. When the patient
request contact between him and the physical therapist he can make an appointment on the day (once a week) the physical therapist is available for tele-consultation. The Habilis
platform also has a forum where patient and physical therapist can communicate with each other. The physical therapist can add extra information by an exercise and the patient
can ask questions about the performance of an exercise and add a video clip (made by the webcam). On the forum the physical therapist posts feedback to the patient, the feedback
will be given on performance (motivational feedback, feedback on the quality of the exercise).
The patients included in the WAD program visit the rehab centre for two days a week, for a period of 8 weeks. On top of the regular treatment they will receive the HABILIS service at
home for one hour a week. The goal of given more treatment at home is to improve the compliance and improve the quality of exercise/training at home. The decision to give more treatment
in regard of less treatment is based on the low frequency the WAD’s patient visit the rehab centre. At the end of the program the WAD patients become 6 hour more therapy then the patients
in the original program.
On top of these home exercises individual teleconsultation sessions can be scheduled in stead of face to face visits for those patients who due to their pain experience problems with
work but who are still working.
In the first and second week of the WAD program, 2 physical therapy sessions of both 2 hours are scheduled. During these sessions two physical therapists are present. One of the
physical therapist teaches half of the group (3 patients) to work with the HABILIS service. Every patient gets about 30 minutes explanation about the HABILIS service in week 1 and 2
by one of the two physical therapists. Just as for all home training exercises, it is a challenge to get and keep the patient motivated. For the HABILIS service this is tried to
be achieved by using positive reinforcement of the physical therapist during the feedback hours and by the HABILIS platform. Besides, if patients do not comply to the exercise
program, they will be contacted repeatedly but without success the treatment will be ended prematurely.
Outcome assessment
Outcome parameters
The main outcome parameters are: compliance with the computer supported exercise program (compliance), satisfaction regarding the computer supported exercise program (user satisfaction),
clinical effect outcomes (clinical effectiveness) and economical benefits of the computer supported exercise program (economic).
The clinical effectiveness is divided in complaints, disability and physical condition. Overall the percentage of responders and non-responders on clinical effectiveness will be
determined. Per patient group (CLBP and WAD) there is a questionnaire to measure complaints and disability and a clinical test to measure the physical condition. The following
measures will be taken:
- Demographic characteristics;
- Compliance exercise program: The tablet PC used by the patient monitors the login data (e.g. login time and login frequency). With these variables the login durations can be calculated per training session and overall;
- Satisfaction, preference & usability: it will be measured by means of a self-constructed questionnaire since no standardized and validated questionnaires are available to assess the user satisfaction, preferences and usability of the treatment, like the tablet PC (Huis in ‘t Veld et al., 2006). The Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh et al., 2003) will be used as the underlying theoretical framework. This model suggests that use behaviour is preceded by performance expectancy, effort expectancy, social influence and facilitating conditions. Therefore, items of the questionnaire will be directed to assessing the patient and the professional’s view on performance expectancy, effort expectancy, social influence, facilitating conditions, and their intention for future computer supported exercise program use/adherence. This will answer the question whether patients and professionals are ready to adopt the service;
- Clinical efficacy factors (subjectively):
- VAS (pain intensity): Pain intensity is assessed by means of VAS scales (Todd, 1996; Gift, 1989). Subjects are asked to rate their experienced level of pain at 1) the present moment, 2) during the past day, 3) during the past week, and 4) maximal pain during the past month. The VAS consists of a 10 cm horizontal line with ‘no discomfort at all’ on the left and ‘as much discomfort as possible’ on the right extremity of the line. Psychometric properties have proven to be sufficient (Jensen & Karoly, 1992).
- Disability:
- Roland Disability Questionnaire (RDQ) for CLBP: Roland Disability Questionnaire for Sciatica (RDQ) (Roland & Morris, 1983) is an illness-specific 24-item functional assessment questionnaire that is frequently used for low back pain. The score, ranging from 0 to 24, reflect a sum of items experienced by the patient. The higher the score the more the patient perceive disability. The RDQ has established validity, reliability and responsiveness to change (Patrick et al., 1995). In this study the Dutch version (Gommans et al., 1997) of the RDQ is used.
- Pain Disability index (PDI) for WAD: The level of subjectively experienced disability is assessed with the Pain Disability index (PDI), a self-rating scale that contains 7 items for the domains: 1) family and home responsibilities, 2) recreation - sports and leisure time activities, 3) social activity - participation with friends and other acquaintances, 4) occupation - activities partly or directly related to working, 5) sexual behaviour – frequency and quality of sex life, 6) self-care – basic life-supporting behaviours and 7) daily activities. Answers are provided on a categorical 11-point scale with ‘not disabled’ and ‘fully disabled’ at the extremes. In a chronic pain population, the psychometric properties of the PDI appeared to be sufficient (Tait et al, 1990).
- Physical condition (objectively):
- CROM test (for WAD): The CROM (Cervical Range Of Motion) instrument is an inter- and intra examiner reliable instrument (S. Love at al. 1998). It measures the range of sagittal (flexion/extension), frontal (lateral flexion) and horizontal (rotation) movements that can be performed by head and neck. The CROM instrument is aligned on the nose bridge and ears and is fastened to the head by a velcro strap. There are three dial angle meters. The sagittal plane meter and the lateral flexion meter are gravity meters. The rotation meter is magnetic and responds to a shoulder-mounted magnetic yoke measuring cervical rotation. Measurements are recorded on a CROM recording sheet. The test is taken at the beginning and at the end of the rehabilitation period.
- Back dynamometry (for CLBP): The back dynamometry is performed by the IsoStation B-200 from Isotechnologies Inc. (Hillsborough, U.S.A). The IsoStation measures isometric end dynamic performance in all three planes of motion: rotation, flexion/extension and lateral flexion. Position, torque and velocity are simultaneously measured in each plane of movement. In the CLBP-group isometric strength, velocity and ROM are measured. First the ROM is measured, than the isometric strength. After that velocity is measured at 25% and than 50% of the maximum isometric strength (a movement is performed 5 times as quick as possible). The ROM is measured for the second time and after that the velocity at 50% and than 25% of the maximum isometric strength (also 5 times as quick as possible).
- VO2max (for CLBP): the VO2max of the CLBP patients will be determined by using the Åstrand ergometer bicycle test (Åstrand and Rodahl, 1986). This is a sub maximal test in which subjects cycle for six minutes at a certain workload. Because it is a sub maximal test it is not valid for measuring maximal oxygen intake, but it is for determining its progress or decline. All subjects start at a workload of 50 Watt. During the first three minutes of the test the hart frequency must climb to at least 120 beats per minute. To reach this hart rate it can be necessary to increase the workload. After the first three minutes the workload will be held. The computer calculates the average hart rate from the fifth and sixth minute. With these measurements the VO2max can easily be estimated with the Åstrand-Ryhming-nomogram. Calculations are corrected for gender, age, length and fat free mass.
- Economic: will be measured by means of a self-constructed questionnaire since no standardized and validated questionnaires are available tot assess the economic. In this self-constructed questionnaire the focus is on the advantages of the computer supported exercise program compared to traditional care practice, the time investments for providing and receiving the computer supported exercise program and potential improvement on the computer supported exercise program.
- Coping: Dutch version of the Coping Strategies Questionnaire, the coping met pijn vragenlijst (CPV). The Dutch version of the Coping Strategies Questionnaire (CSQ) (Spinhoven et al., 1994) was used to assess the extent to which subjects reported the use of coping strategies when they felt pain and consists of 44 items. The main difference between the original CSQ (Rosenstiel & Keefe, 1983) and the Dutch adaptation are the number of items of the behavioural coping subscale (2 for the CPV, and 6 for the CSQ), and the use of a different answering format. Subjects marked 10 cm visual analogue scale with the end point defined in the same way as on the original 7-point Likert-type scale, as “never do” and “always do that”. At the end of the questionnaire, subjects were asked to make two ratings of the overall effectiveness (pain control an ability to decrease pain).
Outcome measures
During the intake of the rehabilitation program the baseline measurement will be conducted. During the baseline measurement, which will take place in vivo (at the clinic), measurements
will be conducted to assess the primary and secondary outcome parameters. Once a week there are multidisciplinary meetings to discuss the progress of every chronic pain patient in
the RRP. In the last weeks of the rehabilitation program the T0 measurements are also performed in vivo (at the clinic).
All subjects will be tested at baseline, immediately after the intervention (T0), at two, four and six month follow-up (T2, T4 and T6). The follow-up measurement can be performed at
the patient home by filling in questionnaires.
The following measures will be taken in the course of the study per patient population and measurements.
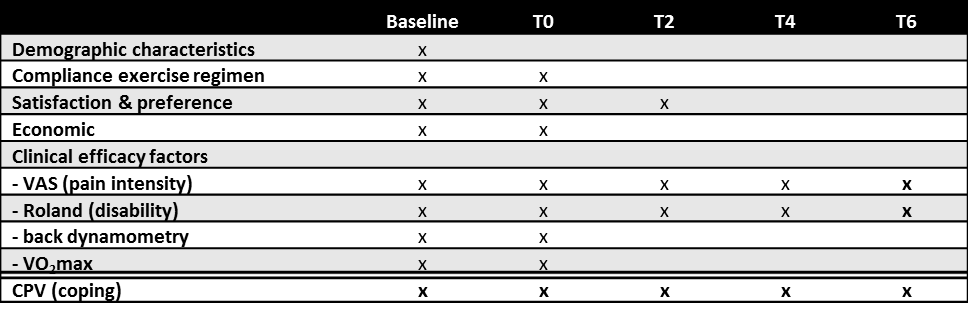
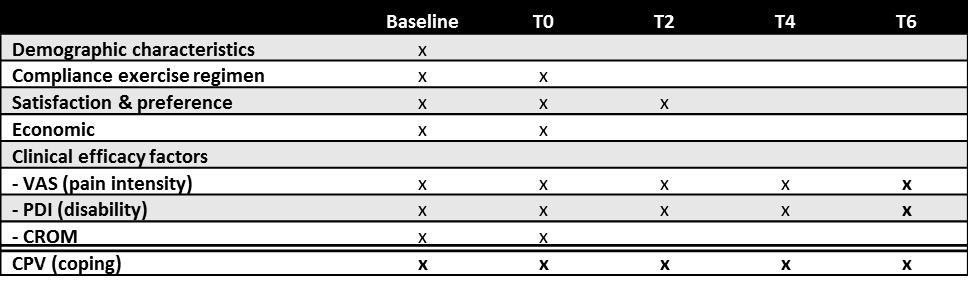
Withdrawal
Subjects can leave the study at any time for any reason if they wish to do so without any consequences. The clinician can decide to withdraw a subject for urgent medical reasons.
Protocol flow chart
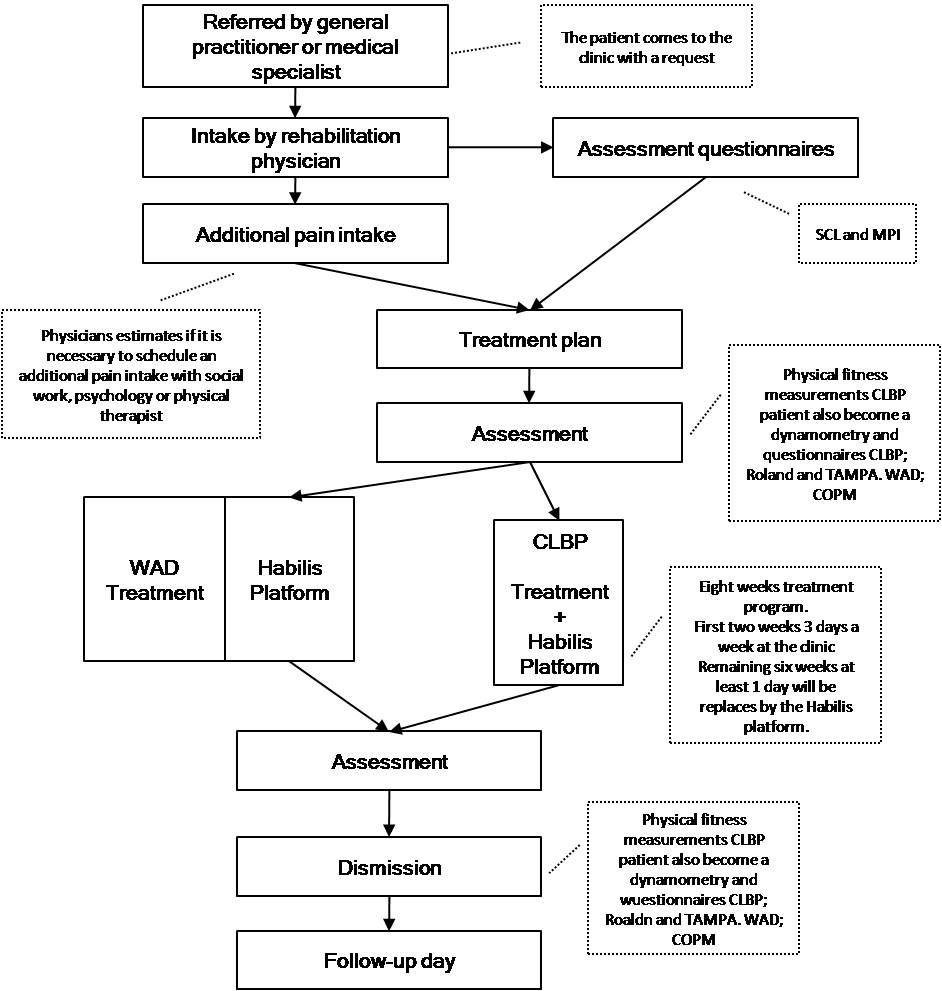
Pulmonary disease - RCR (Stichting Revalidatiecentrum Het Roessingh) [NL]
Description of the scenario
1 - Characterization of the patient
Rick is 55 years old. He is working at a restaurant where he predominantly serves the customers. Rick suffers from chronic obstructive pulmonary disease (COPD), classified as ‘mild - severe’ (GOLD 1-2). Especially during heavy work Rick often experiences shortness of breath, e.g. dyspnoea, associated with panics attacks. Due to the unexpected character of the attacks Rick has become very anxious to perform ‘heavy work’, let alone physical exercises. As a consequence, Rick is avoiding physical activities (e.g. sports, walking, cycling) more and more, eventually ending up in a vicious circle of physical avoidance and deterioration of health status. During a regular consultation with this pulmonologist, the pulmonologist notified his negative vicious circle. Rick was advised to follow a rehabilitation programme in which patients with lung diseases (predominantly COPD) are being treated in groups. The programme is provided by ‘Roessingh Centre for Rehabilitation’, one of the largest rehabilitation centres in the Netherlands. ves these might cause damage to her lower back also. As a consequence, she ended up in a vicious circle of avoidance and pain. Margret’s husband attended her on her pain-related behaviour and advised her to seek help.
2 - Description of the traditional treatment
After an intake consultation with the rehabilitation physician and social worker, Rick was applied for a three-month pulmonary rehabilitation programme during which he has to visit the rehabilitation centre three times a week (about 5-8 hrs duration). During the first month of the programme, he is introduced in the principles of the multidisciplinary rehabilitation programme. The multidisciplinary character of the treatment implies the involvement of a wide variety of therapists (e.g. rehabilitation physician, pulmonologist, physical therapist, sports therapist, social worker, vocational therapist, occupational therapist (on request)). The group has a closed structure. This means the group has the same composition for twelve weeks. The pulmonary rehabilitation program consists of:
- physical therapy: I) information about medication / pulmonary anatomy and physiology, II) breathing exercises related to Activities of Daily Living, III) relaxation exercises.
- sports: individual sport (e.g. Nordic walking, swimming and fitness (endurance, strength)) and team sport (e.g. volleyball, badminton).
3 - Patient Recruitment
After an intake consultation with the rehabilitation physician and social worker, Rick was applied for a three-month pulmonary rehabilitation programme during which he has to visit the rehabilitation centre three times a week (about 5-8 hrs duration). During the first month of the programme, he is introduced in the principles of the multidisciplinary rehabilitation programme. The multidisciplinary character of the treatment implies the involvement of a wide variety of therapists (e.g. rehabilitation physician, pulmonologist, physical therapist, sports therapist, social worker, vocational therapist, occupational therapist (on request)). Due to the fact that Rick has a high travel time to visit the centre he is offered an innovative ‘CLEAR tele-rehabilitation module’ in the second and third month of the three month rehabilitation period. This new module has the advantage that at least one out of the three weekly sessions at the clinic (intramural) can be replaced to Rick’s house (extramural).
4 - Description of the tele-rehabilitation program or the tele-care for the patient
The ‘CLEAR tele-rehabilitation module’ is offered in the second and third month of the three month rehabilitation period. This new module has the advantage that at least one out of the three weekly sessions at the clinic (intramural) can be replaced to Rick’s house (extramural). Rick can decide to exercise whenever and how often he likes with the tele-rehabilitation system. During the session at home, Rick uses the CLEAR platform which he got explained by his physiotherapist during the introduction month in the rehabilitation centre.
5 - Description of a tele-reabilitation session
Today, Rick agreed with his therapist to execute some of the breathing exercises he learned at the clinic by means of the CLEAR tele-rehabilitation system. He starts up his computer and logs in with his personal identification code and password. Rick can choose from the exercises which are selected by the physical therapist. He starts with watching an instruction video about breathing exercises related to Activities of Daily Living. Thereafter, he practices for himself in different body positions (e.g. lying, sitting, standing, walking, cycling and walking stairs). A webcam is incorporated in the system, so exercises in the lying, sitting and standing position are recorded by the CLEAR system and can be discussed by means of videoconference with the physical therapist. Feedback will be given on performance (motivational feedback, feedback on the quality of the exercise) and questions from the patient. Therefore an appointment is made for ten minutes once a week.
6 - Description of the interaction with the therapist
A webcam is incorporated in the system, so the exercises can be recorded by the CLEAR system and discussed with the physical therapist by means of videoconference. Feedback will be given on performance (motivational feedback, feedback on the quality of the exercise) and questions from the patient. Therefore an appointment is made for ten minutes once a week.
7 - Description of the therapist session
The therapist connects to the platform and examines the performances of the patient in the previous sessions. He or she assigns exercises for the next week related to the results obtained so far. During the ten minute appointment with the patient the therapist logs into the system and talks to the patient by means of videoconference.
8 - Description of the advantages the programs has for the patients
Thanks to this remote treatment, the patient has had the opportunity to continue seeking a personalized and individualized therapy schedule by a therapist tailoring the treatment to their specific deficits without having to afford transportation or wasting time traveling to the rehabilitation centre.
9 - Description of the advantages this program has for the therapist
The therapist can establish an individualized treatment for the patient, saving time and money. The therapist gets a better idea of what the patients are doing at home in relation to their disease.
Clinical Protocol
Here below the protocol on COPD designed by RCR (Rehabilitation Centre Het Roessingh) is described.
Overview
Chronic obstructive pulmonary disease (COPD) is a chronic progressive disease. COPD is characterized by constriction of the bronchia resulting in respiration constrain,
complains like coughing and shortness of breath are common for COPD patient. Smoking is the most important factor by the development of this disease. COPD can manifest
itself just 10 years after the smoking addiction started (Fabbri et al., 2003). The prevalence of COPD by men slightly decreased last years, by women the prevalence increased
because of the increases of smoking prevalence by women. In the next 10 years the COPD prevalence of men will remain the same, the COPD prevalence of women will increase.
Due to aging the amount of COPD patients will increase (Feenstra et al., 2001). Patient over the age of 45 are at risk for COPD. COPD is predominantly in the lower socio-economic
classes. A lower socio-economic class refers to a lower education- and income level (Tabak & Smit, 2001). The physical capacity of patients with serious COPD is often limited
through reduced muscle-and nutritional condition. The strength and physical condition of the respiratory and skeletal muscles of COPD patients is often decreased.
The HABILIS service will partly replace the outpatient rehabilitation of the COPD GOLD classification II/III treatment by home training. The rationales for doing this are multiple:
it will contribute to a reduction of costs; it enables patients to more easily translate the learned skills to every day life; it fits in the current trend of self management of
the patient and it enables patients to exercise much more at moments preferred by the patient and as such makes treatment at least as or even more effective than traditional care.
To get insight in whether these aims are being fulfilled each individual patient is monitored on time needed by professionals in the new way of care provision and by changes in
health outcome achieved during treatment with the HABILIS service as partly replacement of traditional care.
In the COPD GOLD classification III/IV group the HABILIS service will be an additional treatment. The rationale for using it here as an additional treatment is that these patients
come to the rehab centre already at a minimum amount, caused by the fact that their capacity is to low to come more often. The hypothesized advantages of the HABILIS service are:
it will contribute to the quality of the treatment, also because elements of the treatment are being repeated more often; it enables patients to more easily translate the learned
skills to every day life; it fits in the current trend of self management of the patient; it enables patients to exercise much more at moments preferred by the patient and as such
makes treatment at least as or even more effective. Whether it indeed makes treatment more effective will be monitored in each individual patient by monitoring their changes in
health outcome.
Target Patient Group
Population (base)
Participants receiving an outpatient rehabilitation program at Clinical Centre for patients with pulmonary diseases COPD/ASTMA (Chronic Obstructive Pulmonary Disease):
- # COPD Gold Classification II (mild) and III (serious)
- # COPD Gold Classification III (serious) and IV (very serious)
Inclusion criteria
The inclusion criteria are:
- pulmonary diseases (COPD Gold Classification II/III/IV);
- capable of following outpatient treatment (2 or 3 days per week);
- motivated;
- non smoking;
- familiar to pulmonary specialist.
Exclusion criteria
The exclusion criteria are:
- insufficient understanding of the National language;
- iBMI > 35;
- age <18 years.
Admission and baseline assessment
The patient is referred by the pulmonologist. Together with their partner the COPD patient is invited for an intake with the rehabilitation physician and the social worker.
Both intakes take 30 minutes and are planned on one day. Immediately after the intakes these specialists discuss the patient. The patient receives the result of this intake
immediately. When the result of the intake is positive the nurse gives information about the treatment.
At the start of the treatment the social worker interviews the patient about the Chronic Respiratory Questionnaire (CRQ).
The CRQ is a disease specific questionnaire of quality of life. The parts of the CRQ to be questioned are: fatigue, shortness of breath,
emotion and experience. During the first multidisciplinary meeting the social worker explains the CRQ results. Every patient included in
the pulmonary rehabilitation program participates in the HABILIS service. Patients who get information from the site or elsewhere and who
are interested in the HABILIS service can involve in the program by following the same procedure as is described above.
The baseline measurement coincides with the intake of the rehabilitation program.
Treatment protocol
The computer supported exercise program is a home based exercise program supported by technology for patients with a chronic disease. The computer supported exercise program
consist of a tablet pc with webcam and with new developed software giving access to a database of exercises and different communication tools (like a webcam) to facilitate
contact between the patient and professional. With the computer supported exercise program the therapist composes a tailored home based exercise program for his patient.
The patient can execute the program on a self-scheduled time. Every week the patient records 2 or 3 exercises with the webcam to be assessed by the therapist. Patient and
professional can contact each other by email, chat, phone or tele-conference (with the webcam). The therapist monitors the patient and once a week, at a fixed time, he will
contact the patient by one of the modalities to answer possible questions of the patient about the tailored exercise program and to review the recorded exercises. The
therapist can add and delete exercises on the exercise program of the patient during the rehabilitation.
Subjects will receive the rehabilitation program extended with the computer supported exercise program. During eight to twelve weeks the patient visits the rehabilitation
centre two or three times a week to participate in different therapies; physical therapy, condition training and sports, occupational therapy and swimming. The computer
supported exercise program consist of a tele treatment service with a database of exercises video files and offers different modalities (email, chat, and video-conference)
to allow for contact between patient and professional. This telemedicine application is an opportunity for the patient to train at home supervised and monitored by his
therapist to increase his physical condition. The computer supported exercise program will be implemented in the rehabilitation program for COPD/ASTMA in two different ways:
- Partial replacement of the traditional rehabilitation program: within the 3-days rehabilitation program (COPD/ASTMA: GOLD II+III) the application will be used as a replacement of 1 day treatment at the clinic. During the first part of the rehabilitation (first 2-4 weeks) the patients will visit the clinic 3 days a week to receive their rehabilitation program. They will also be trained in using the computer supported exercise program. During this period a tablet PC will be installed at the patients’ home. After this period the patient visits 2 days per week the clinic to receive his rehabilitation program and execute his tailored exercise program at home till the end of the rehabilitation program. The therapist is available for contact during the two days at the clinic and a scheduled time on the replaced day;
- Complementary to the traditional rehabilitation program: within the 2-days rehabilitation program (COPD/ASTMA: GOLD III+IV) the application will be used as complement to the 2 days treatment at the clinic. During the first part of the rehabilitation (first 2-4 weeks) the patients will come 2 days to the clinic to receive their rehabilitation program. They will also be trained in using the computer supported exercise program. During this period a tablet PC will be installed at the patient home. After this period the patient remains to come 2 days to the clinic to receive their rehabilitation program and will execute their tailored exercise program at home until the end of the rehabilitation program. The therapist is available for contact during the two days at the clinic at scheduled times within the week.
The agenda function of the HABILIS application gives the patient the opportunity to schedule the exercise program through the week. In addition patients have the opportunity to view the exercises on their tablet pc by playing the video-files. Every week the patient records 2 or 3 exercises with the webcam to be assessed by the therapist. Also the patients are offered an email, chat and tele-consulting function (with the webcam) on the tablet pc from which they can contact their therapist in case they have questions about their exercises. Patients can support their questions with a video of their execution of the exercise. Once a week, at a fixed time, the therapist will contact the patient by one of these modalities and give the patient feedback about the compliance to the exercise schedule and the exercise performance.
During the stay in the Centre
The duration of the program is three months. Every month the program is being repeated. So every treatment element is being applied three times. The group has an open structure which means that each month ‘new’ patients are allowed to enter the group. During the first month of the program, the patient is introduced to the multidisciplinary rehabilitation program. The multidisciplinary character of the treatment implies the involvement of different therapists (e.g. rehabilitation physician, pulmonologist, physical therapist, sports therapist, social worker, vocational therapist, occupational therapist (on request)). In the last two weeks of the first month of the program there will be scheduled two extra hours for learning to work with the HABILIS service. During these meetings the physical therapist explains the HABILIS platform and enables the patient to practice with the HABILIS service. Through education / explanation of the platform the patient gets motivated to exercise. At the start of the program patients sign a paper that they will participate in the program with optimal motivation.
Remotely
The patients in both the intensive and the low intensive group will be able to use the HABILIS service at home during the second and third month of the three month rehabilitation period.
In order to make it easier for the patient he or she will receive a HABILIS service user manual. In the intensive group at least one out of the three weekly sessions at the clinic
(intramural) will be replaced by home exercising. In the low intensive group no clinical sessions will be replaced by home exercising. Home exercising is only additional.
In both groups the physical therapist selects exercises which are suitable for the patient. Together with the patient he or she schedules what, when and where the patient will
practice. All this will also be printed on paper, which will be used as a guide for home training. At the request of either the therapist or the patient a videoclip of an exercise
can be made with an incorporated webcam at the patients’ home. In this way the therapist can review the exercises. On a weekly basis the physical therapist and the patient have time
to discuss the home training program and update it when necessary. This will take place at the clinic. Besides this the therapist will be available for feedback (by phone, e-mail or
videoconference) for two hours a week on days the patient practices at home. Patient and therapist make appointments on when to log in for feedback on the exercises. The HABILIS
service will be used for the duration of the traditional pulmonary rehabilitation, starting in the second month of the rehabilitation (so for 2 months).
Just as for all home training exercises, it is a challenge to get and keep the patient motivated. For the HABILIS service this is tried to be achieved by using positive reinforcement
of the physical therapist during the feedback hours and by the HABILIS service. Besides, if patients do not comply to the exercise program, they will be contacted repeatedly but
without success the treatment will be ended prematurely.
Outcome assessment
Outcome parameters
The main outcome parameters are: compliance with the computer supported exercise program (compliance), satisfaction regarding the computer supported exercise program (user satisfaction),
clinical effect outcomes (clinical effectiveness) and economical benefits of the computer supported exercise program (economic).
The clinical effectiveness is divided in complaints, disability and physical condition. Overall the percentage of responders and non-responders on clinical effectiveness will be
determined. Per patient group (COPD/ASTMA) there is a questionnaire to measure complaints and disability and a clinical test to measure the physical condition. The following measures
will be taken:
- Demographic characteristics;
- Compliance exercise program: The tablet PC used by the patient monitors the login data (e.g. login time and login frequency). With these variables the login durations can be calculated per training session and overall;
- Satisfaction, preference & usability: it will be measured by means of a self-constructed questionnaire since no standardized and validated questionnaires are available to assess the user satisfaction, preferences and usability of the treatment, like the tablet PC (Huis in ‘t Veld et al., 2006). The Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh et al., 2003) will be used as the underlying theoretical framework. This model suggests that use behaviour is preceded by performance expectancy, effort expectancy, social influence and facilitating conditions. Therefore, items of the questionnaire will be directed to assessing the patient and the professional’s view on performance expectancy, effort expectancy, social influence, facilitating conditions, and their intention for future computer supported exercise program use/adherence. This will answer the question whether patients and professionals are ready to adopt the service;
- Clinical efficacy factors (subjectively):
- Complaints VAS (pain intensity): Pain intensity is assessed by means of VAS scales (Todd, 1996; Gift, 1989). Subjects are asked to rate their experienced level of pain at 1) the present moment, 2) during the past day, 3) during the past week, and 4) maximal pain during the past month. The VAS consists of a 10 cm horizontal line with ‘no discomfort at all’ on the left and ‘as much discomfort as possible’ on the right extremity of the line. Psychometric properties have proven to be sufficient (Jensen & Karoly, 1992).
- Disability (CRQ): The Chronic Respiratory Disease Questionnaire (CRQ) is a widely used instrument in respiratory rehabilitation. CRQ is an interviewer administered questionnaire, which asks patients to rate their health status (physical and emotional) in four domains: dyspnoea, fatigue, emotional function, and mastery COPD/ASTMA (Guyatt et al., 1987). Domain and total scores are presented on a Likert-type scale from 1 (most severe impairment) to 7 (no impairment). Is this study we use the Dutch translation of the CRQ (Wijkstra et al., 1994).
- Physical condition (objectively):
- Six-minutes walk test (6MWT): The six-minute walk test is generally used at the start of a Pulmonary Rehabilitation program and/or in the evaluation of a lung transplant. The results of the test are helpful in setting up an exercise program that is designed to meet the patient’s needs. The object of this test walks as far as possible for 6 minutes on a flat surface such as a hallway. During the test patients are permitted to slow down, to stop, and to rest if necessary;
- Hand grip strength: The hand grip strength of the COPD/ASTMA patient will be measured with the Jamar Dynamometer. During measurement the patient seats on a chair (without armrest), elbow flexed about 90° and wrist in neutral to slight ulnal deviation. The Jamar Dynamometer is set in second position on all tests. Each participant will be instructed about the Jamar, told to grip maximally, and then rest, first with the right hand, then the left, three consecutive times. The reliability and validity of the Jamar has been stressed and has been found to be the standard of objective grip strength measurements (Harkonen et al., 1993).
- Economic: will be measured by means of a self-constructed questionnaire since no standardized and validated questionnaires are available tot assess the economic. In this self-constructed questionnaire the focus is on the advantages of the computer supported exercise program compared to traditional care practice, the time investments for providing and receiving the computer supported exercise program and potential improvement on the computer supported exercise program.
Outcome measures
During the intake of the rehabilitation program the baseline measurement will be conducted. During the baseline measurement, which will take place in vivo (at the clinic), measurements
will be conducted to assess the primary and secondary outcome parameters. In the last weeks of the rehabilitation program the T0 measurements are also performed in vivo (at the clinic).
All subjects will be tested at baseline, immediately after the intervention (T0), at two, four and six month follow-up (T2, T4 and T6). The follow-up measurement can be performed at the
patient home by filling in questionnaires.
The following measures will be taken in the course of the study per patient population and measurements.
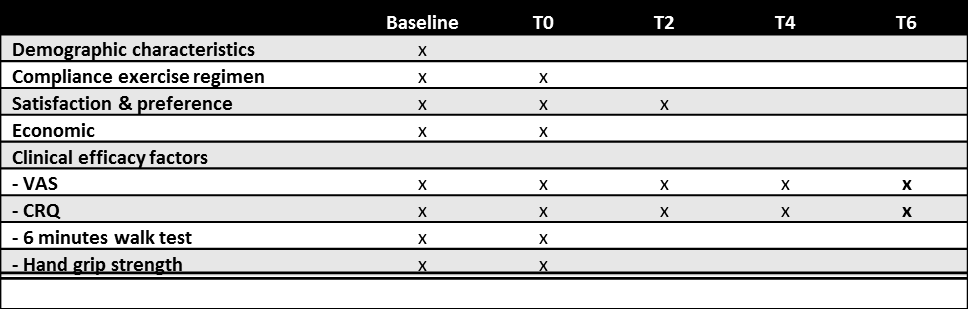
At the start and the end of the treatment the social worker interviews the patient about the Chronic Respiratory Questionnaire (CRQ). The CRQ is a disease specific questionnaire of quality of life. The parts of the CRQ to be questioned are: fatigue, shortness of breath, emotion and experience. At the end of the treatment the social worker also measures the personal experience of the COPD patient through questions. This is a subjective measuring. During the first multidisciplinary meeting the social worker explains the CRQ results. Every patient of the group is once a week discussed during the multidisciplinary meeting of clinicians and the pulmonologist. Every COPD patient has a 10 minutes consultation with the pulmonologist once every two weeks.
The baseline measurement coincides with the intake of the rehabilitation program. All subjects will be tested at baseline, immediately after the intervention (T0), at two, four and six month follow-up (T2, T4 and T6) if possible within the timeframe of the CLEAR project.
Withdrawal
Subjects can leave the study at any time for any reason if they wish to do so without any consequences. The clinician can decide to withdraw a subject for urgent medical reasons.
Protocol flow chart